BC EMALB Practical Examination Guidelines
.jpg)
The Canadian Red Cross, BC Ambulance Service and BC Emergency Medical Assistant's Licensing Branch follow the National Occupational Competency Profile (NOCP) for most EMR skills, as endorsed by the Paramedic Association of Canada (PAC). EMALB, the agency responsible for Licensing evaluations in British Columbia, has additional, sometimes contradictory requirements to successfully complete their practical scenario examinations. These requirements are outlined in the EMALB British Columbia Provincial Examination Guidelines booklet. Whenever the BC EMALB Examination Guidelines contradict or supplement the information provided in the Canadian Red Cross Emergency Care for Professional Responders text book, the EMALB Examination Guidelines take precedence and overrule any other interpretations.
The Emergency Medical Assistants Licensing Board British Columbia Provincial Examination Guidelines for Primary Care Paramedics and Emergency Medical Responders is produced and updated by the BC EMALB team of medical professionals and advisors. The purpose of the Guidelines document is provide insight and consistency for Emergency Medical Responder and Primary Care Paramedic course students preparing for their EMALB practical scenario evaluations.
It is important to note that the BC EMALB Provincial Examination Guidelines include skills and protocols at the Primary Care Paramedic (PCP) level as well as the Emergency Medical Responder (EMR) level. Take care to differentiate the PCP only components when reviewing the Examination Guidelines for purposes of preparing for practical scenario Licensing evaluations at the Emergency Medical Responder level. It would be inappropriate to implement PCP level skills and decisions during EMR examinations, and this would likely result in an unsuccessful result.
For the most part, the EMALB Examination Guidelines for EMR skills follow the same protocols, principles and processes as those outlined by the Canadian Red Cross and PAC NOCP. However, there are a few specific Examination Guidelines which differ slightly from the National PAC NOCP, which means you need to be aware of them for BC EMALB EMR Licensing purposes. The EMALB British Columbia Provincial Examination Guidelines that are particularly relevant to Emergency Medical Responders in British Columbia are listed in detail below, on this page.
These specific Examination Guidelines include:
- NEXUS Spinal Motion Restriction Decision Matrix
- Determining Cardiac Arrest for Hypothermic Patients
- Maximum AED Shocks for Hypothermic Patients
- Pediatric Pulse Oximetry
- Realignment of Grossly Deformed Limbs
- Sager Traction Splint
- Treatment of Open Chest Wounds (Pneumothorax)
- Treatment of Burn Injuries
- Assessment of Stroke & TIA
- Administering Medications in BC
- Administration of Glucogel to an Unresponsive Patient
- Administration of Entonox for Pain Management
- Administration of Nitroglycerin with or without a Prescription
- Administration of ASA before Vital Signs
- Administration of Naloxone for Opioid Overdose
Updates to the EMALB Examination Guidelines
.jpg)
BC EMALB does update their examination guidelines, and the corresponding treatment protocols required to meet Licensing requirements, on a regular basis without advance notice. It's definitely a good idea to revisit and review the most current version of the Examination Guidelines as you prepare for your EMALB Emergency Medical Responder or Primary Care Paramedic practical scenario exams.
The cover page of the Examination Guidelines booklet states that these guidelines were produced by the Ministry of Health in 2019. However the bottom right footer on the interior pages shows the date of the most recently published version (ie..."Current July 27, 2022"). Checking the footer date can help you determine if any significant changes may have been implemented in the time since your most recent certification training.
If you completed your most recent Emergency Medical Responder certification training course prior to the updates listed below, you should definitely revisit these skills and topics before completing your upcoming BC EMALB written and practical examinations. Many of these topics are covered in more detail throughout Medi-Pro's EMR Study Guide, EMR Cheat Sheet, and other online resources on Medi-Pro's website.
Recent EMR level updates to the EMALB Examination Guidelines:
July 27, 2022
- As of July 27th, 2022 the EMLAB Examination Guidelines stipulate that the minimum Systolic Blood Pressure to administer 0.4 mg of Nitroglycerin is 110 mmHg. This now applies both to patients with a previous Nitro prescription and those without a previous Nitro prescription. Previous versions of the EMALB Examination Guidelines asserted a minimum Systolic of 90 mmHg for patients with a prescription, and 100 mmHg for patients without a prescription.
- As of July 27th, 2022 the EMLAB Examination Guidelines stipulate that when transporting patients with Full SMR precautions or Partial SMR precautions, the head of the stretcher/cot should be raised 30°. Previous versions of the EMALB Examination Guidelines asserted that the head of the cot should be raised 30° only when traumatic head/brain injury was suspected.
- As of July 27th, 2022 the EMLAB Examination Guidelines stipulate that a maximum of 3 defibrillation shocks should be delivered when performing CPR on a Hypothermic patient. After the third defibrillation shock is delivered to a Hypothermic patient, rescuers should ignore subsequent AED prompts for analysis or shock and simply continue with CPR compressions and ventilations as appropriate.
March 16, 2022
- As of March 16, 2022 the EMLAB Examination Guidelines require cooling burns for 15-20 minutes, whereas the previous versions indicated that on-scene burn cooling time should be limited to 1-2 minutes.
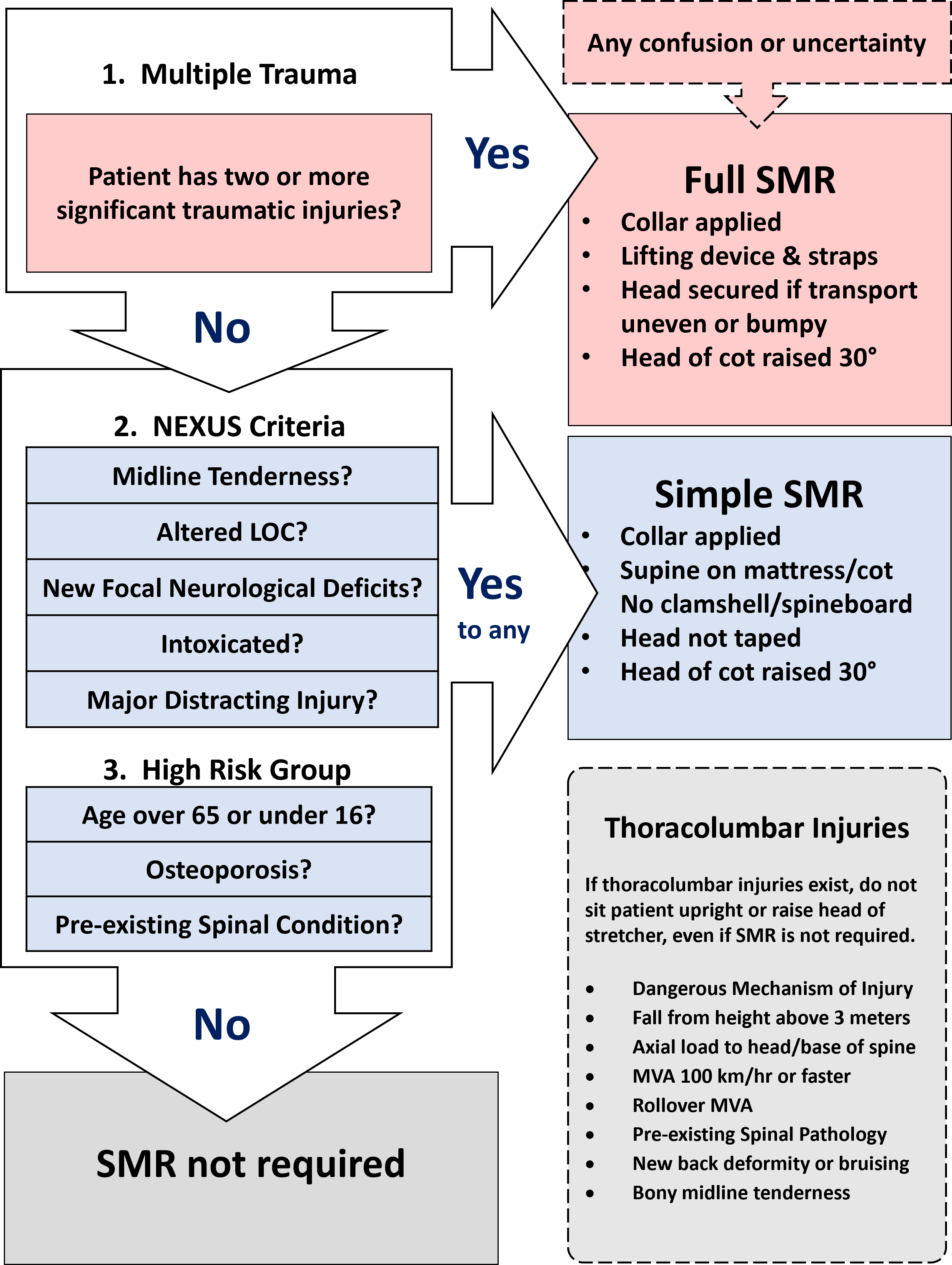
NEXUS Spinal Motion Restriction
.jpg)
A significant portion of your EMR training course involves learning and practicing the prinicples of Spinal Motion Restriction (SMR), the Canadian C-Spine Rules, and the National Emergency X-Radiological Utilization Study (NEXUS) protocols which replaced the older Spinal Immobilization approach. The new SMR guidelines and accompanying modified NEXUS protocols adopted by BC EMALB provide paramedics with more options and flexibility to provide patient care when spinal cord injury is suspected, but the complex decision matrix requires memorization and practice.
What the EMALB Examination Guidelines say:
- Follow the NEXUS Criteria
Contradictory information in the Emergency Care for Professional Responders text book:
- The Canadian Red Cross Emergency Care text book indicates that the “Canadian C-Spine Rules” should be followed for determining when and what type of Spinal Motion Restriction (SMR) is appropriate.
What this means for Emergency Medical Responders in BC:
- Emergency Medical Responders in British Columbia will need to be familiar with the NEXUS / Modified NEXUS SMR Decision Matrix for determining when SMR measures are appropriate.
- The NEXUS decision criteria regarding Spinal Motion Restriction (SMR) measures should be applied whenever the mechanism of injury is suggestive of potential spinal cord injury.
- Based on the the NEXUS / Modified NEXUS SMR Decision Matrix Emergency Medical Responders in British Columbia will apply either Full SMR measures or Simple SMR measures as appropriate for the patient and circumstances.
- Full SMR includes applying a properly sized cervical immobilization collar, and strapping the patient to a Robertson Orthopedic/Clamshell Stretcher with support cushions on both sides of the head. When Full SMR is utilized, the patient's head should be secured directly to the stretcher when effecting a technical rescue such as high-angle, over-the-bank, or confined space.
- Simple SMR involves applying a properly sized cervical immobilization collar, and positioning the patient supine on a mattress or cot. Although a lifting device such as a clamshell stretcher or spineboard may be necessary to move the patient onto the cot, these devices are not required during transport and may be removed from under the patient after they've been placed on the cot.
- When transporting patients with either Full SMR or Simple SMR, the head of the cot should be raised 30°.
- Emergency Medical Responders in British Columbia will also make decisions about patients for whom SMR is not indicated, but may have Thoracolumbar Injuries.
- In instances of non-SMR Thoracolumbar Injuries, the patient should be transported without sitting up or raising the head of the stretcher.
NEXUS SMR Decision Matrix for Injuries with Spinal Mechanism
Determining Cardiac Arrest for Hypothermic Patients
.jpg)
As Hypothermia progresses from mild, to moderate and eventually to the severe category, the body's metabolic process can slow to an almost imperceptible rate. This can make it challenging to definitively determine the presence or absence of a carotid pule, prior to begining CPR-AED protocols when the patient is not breathing and appears otherwise lifeless. The heart could still be beating, just at a rate and strength that makes it difficult to detect. For this reason, you should take a bit of extra time and care when performing your Primary Assessment, particularly the Airway, Breathing, and Circulation check if hypothermia is known or suspected to be a factor.
What the EMALB Examination Guidelines say:
- Take up to 30-45 seconds to determine pulselessness in the severely hypothermic patient.
Contradictory information in the Emergency Care for Professional Responders text book:
- The Canadian Red Cross Emergency Care text book states that up to 60 seconds should be taken to assess the pulse of a patient with suspected Hypothermia.
What this means for Emergency Medical Responders in BC:
- Emergency Medical Responders in British Columbia should assess the pulse of a patient with suspected Hypothermia for no more than 45 seconds, and begin CPR-AED protocols if no pulse is detected in that that time.
AED Shock Limits for Hypothermic Patients
.jpg)
When performing Basic Life Support level CPR and following Automated External Defibrillation (AED) protocols on a patient who is significantly/severely hypothermic, the AED may become less effective than normal. At a certain point, the time spent interrupting compressions to allow the AED to analyze the heart rhythm for Ventricular Tachycardia or Ventricular Fibrillation may hamper rescuscitation efforts, with a dimishing chance of positive outcomes. The relatively small chance that the AED shock will result in return of spontaneous circulation (ROSC) is no longer sufficient to justify the loss of coronary perfusion pressure (CPP) during pauses in compressions.
What the EMALB Examination Guidelines say:
- In the event of cardiac arrest apply AED and analyze, defibrillate up to three times if indicated, continue with CPR and rapid transport to the hospital. (After three defibrillations, do not pause CPR for analyzing or shocks)
Contradictory information in the Emergency Care for Professional Responders text book:
- The Canadian Red Cross Emergency Care text book does not provide information or guideance specific to the performance of CPR and/or limitations to the use of an AED on a Hypothermic patient.
What this means for Emergency Medical Responders in BC:
- Emergency Medical Responders in British Columbia should initially utilize an AED as normal when performing CPR on a hypothermic patient, however once 3 defibrillation shocks have been delivered, the AED should be ignored and rescuers should no longer interrupt chest compressions to allow the AED to analyze or deliver subsequent shocks. At that time, the rescuers should consider Treatable CPR criteria and potentially continue CPR in transport.
Pediatric Pulse Oximetry
The use and interpretation of a finger-tip pulse oximeter to measure a peripheral capillary oxygen saturation (SpO2) can provide valuable information about a patient's current condition, as well as benchmarks to determine if the patient's condition is improving or declining overall. As with any electronic device, there are limitations to the accuracy of pulse oximters, and certain conditions can compromise the accuracy of the data displayed. Sickle cell anemias, carbon monoxide poisoning, poor peripheral perfusion, and dirty/painted fingernails are examples of conditions which can cause a pulse oximeter to malfunction. When rescuers utilize a pulse oximeter it is important to rely on all the data available and to treat the patient appropriately to their overall condition, not just the readings of a single device.
What the EMALB Examination Guidelines say:
- The use and/or interpretation of a pulse oximeter is Contraindicated for pediatric patients weighing less than 10kg (22lbs).
Contradictory information in the Emergency Care for Professional Responders text book:
- The Canadian Red Cross Emergency Care text book does not provide direction for the use of a pulse oximeter based on age or weight. The text book does outline other limitations of a pulse oximeter, but not specifically regarding the age or weight of the patient being assessed.
What this means for Emergency Medical Responders in BC:
- When Emergency Medical Responders in British Columbia are assessing and/or providing care for pediatric patients weighing less than 10 kilograms (22 pounds), they should not utilize a pulse oximeter or make clinical decisions based on pulse oximetry data. In many cases, the rescuers will need to make an unverified determination of weight and take action appropriate to their best estimate.
- At all times, and especially when dealing with pediatric patients, the data provided by a pulse oximeter should be regarded as possibly less than completely accurate or reliable.
Realignment of Grossly Deformed Limbs
.jpg)
The term "Gross Deformity" refers to a fracture or dislocation which, in addition to causing the pain and surrounding tissue damage typically associated with an injury of this type, has distorted the limb or extremity far beyond its normal anatomical position. This can cause other complications such as a lack of circulation distal to to the injury, which creates an urgent limb-threatening injury, and can render patient packaging and transport impractical or even impossible.
What the EMALB Examination Guidelines say:
- Absence of distal circulation may indicate a limb-threatening injury or condition.
- Attempt realignment to anatomical position once if limb is found to be pulseless, or if needed to facilitate transport.
- Manage the patient as unstable and initiate rapid transport if distal circulation cannot be restored.
Contradictory information in the Emergency Care for Professional Responders text book:
- The Canadian Red Cross Emergency Care text book states that a single attempt may be made to straighten a fractured limb only if more advanced medical care is not available within 30 minutes.
What this means for Emergency Medical Responders in BC:
- Emergency Medical Responders in British Columbia will make a single attempt to realign a limb that is grossly deformed if circulation is compromised distal to the injury, or if the deformity makes transport impractical.
- A pulseless limb is a "limb-threatening" injury and urgent transport should be initiated if realignment does not restore circulation.
- This is regardless of distance to medical care.
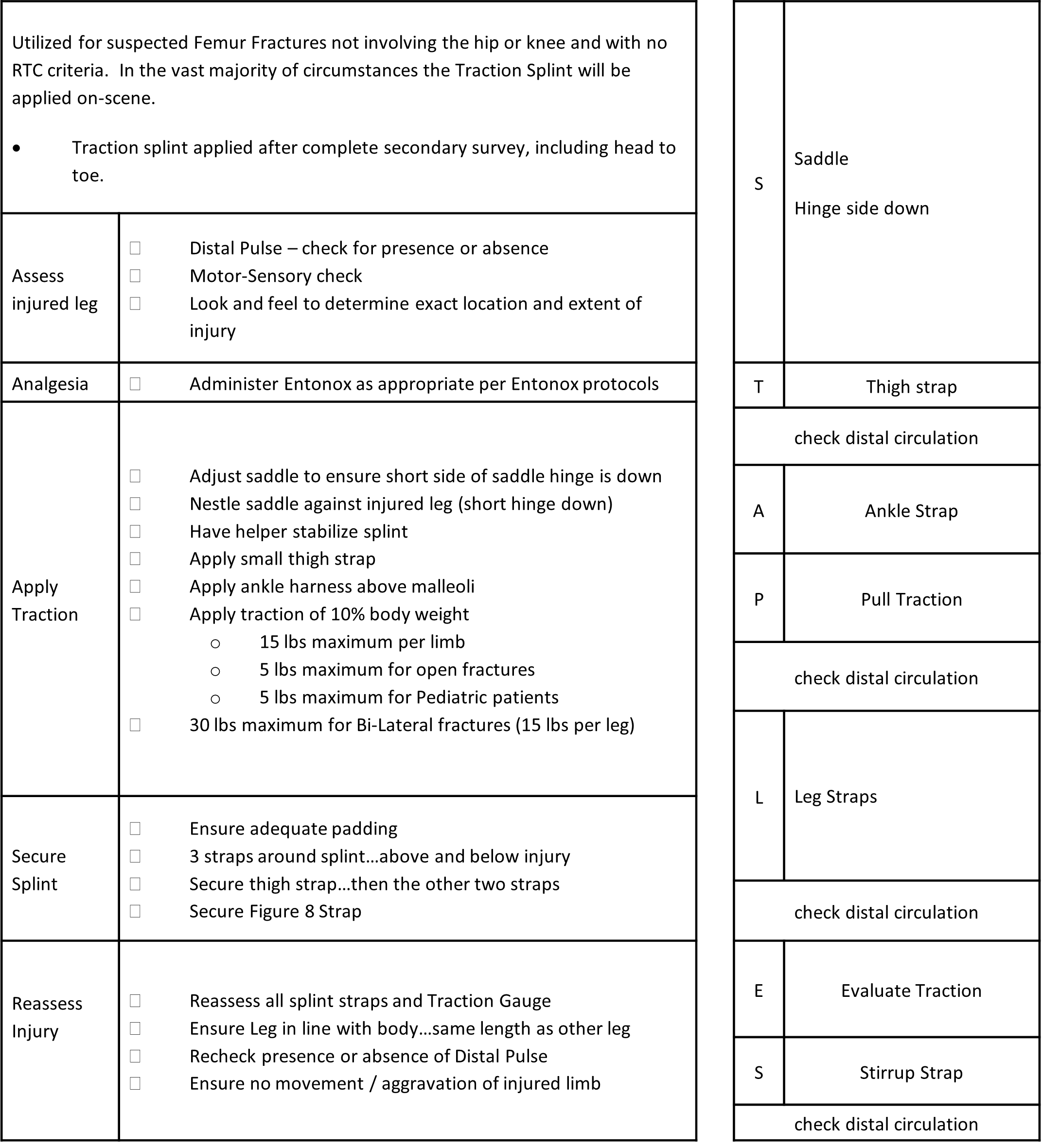
Sager Traction Splint
.jpg)
When properly applied, a traction splint can alleviate much of the pain from a femur fracture as well as preventing further interal tissue and blood vessel trauma by holding the fractured bone ends from grating against or sliding further alongside each other. The Sager traction splint is preferred by BCEHS and will be provided during EMALB Licensing evaluations, so examination participants must be proficient with this specific brand and EMALB's specifications for it's application. Optimal patient care when utilizing a SAGER Traction Splint also involves careful stabilization of the injury throughout application, judicious placement of securing straps and adequate padding to ensure there are no hot spots or excessive movement on the affected leg. Transport of a patient wearing a traction splint will usually involve placement of a Robertson Orthopedic Stretcher (Clamshell) under the patient prior to lifting onto the cot.
What the EMALB Examination Guidelines say:
Traction Splint Indications
- Suspected mid-shaft femur fractures
Procedure
- Assess distal circulation, sensation, and function.
- Apply cold, if appropriate and distal circulation is not impaired.
(ice on for 10 minutes, off for 5) - Give analgesia (Entonox) if not contraindicated.
- Ensure that patient is supine with the injured leg in line with the body.
(maintain manual stabilization of the injured leg throughout and after movement) - Reassess distal pulse
- Place traction splint beside injured leg.
- Secure thigh strap/bandage.
- Apply ankle harness above the malleoli.
- Apply traction (once traction is applied, do not release traction)
a) Closed, mid-shaft femur fracture: 10% of patient's body weight to a maximum of 15 lbs.
b) Open, mid-shaft femur fracture: Maximum 5lbs. - Reassess distal pulse.
- Ensure adequate padding between splint and injured leg.
- Stabilize injured limb and splint by applying three elasticized straps.
- Reassess distal circulation, sensation, and function.
- Traction should be reassessed and corrected if necessary with each movement/reassessment of ABC’s or vitals.
Contradictory information in the Emergency Care for Professional Responders text book:
- The Canadian Red Cross Emergency Care text book speaks to utilizing traction splints in general principles, without identifying a specific brand of traction splint or procedure for application. Sager traction splint manufacturer's instructions include applications for mid-third femur fractures and tibial/fibial fractures, however EMALB Examination Guidelines restrict the parameters to mid-third femur fractures only.
What this means for Emergency Medical Responders in BC:
- Emergency Medical Responders preparing for EMALB Licensing examinations should be familiar and comfortable with the Sager traction splint specifically, and limit its application to mid-third femur fractures only.
- The ideal and most common circumstances where a Sager traction splint will be utilized is a mid-third femur fracture with no additional or accompanying life-threatening conditions.
- If the patient has any immediate life-threatening conditions such as reduced level of responsiveness or significant shock, the traction splint is considered too time consuming and urgent transport with basic stabilization is more appropriate.
- In general, if the Sager traction splint is not applied on-scene it will not be utilized during transport either.
- The administration of Nitrous Oxide (Entonox) as an analgesic prior to applying traction will generally make the patient more comfortable and the traction more effective. However, if Entonox is contraindicated, the the traction splint can still be applied.
- Emergency Medical Responders may find the acronym "S-T-A-P-L-E-S" useful in remembering the procedure to apply a Sager traction splint.
Sager Traction Splint Mnemonic (STAPLES)
- S – Saddle placed against ischial tuberosity, hinge-side down
- T – Thigh strap (narrow webbing) secured around upper thigh through saddle
(reassess limb for distal circulation, sensation and function after securing thigh strap) - A – Ankle strap secured above malleolus/malleoli (ankle bone)
- P – Pull traction appropriate to body weight and injury (1 lb per pound of body weight to a maximum of 15 lbs traction; maximum 5 lbs traction for open fracture)
(reassess limb for distal circulation, sensation and function after pulling traction) - L – Leg straps secured above and below fracture, and around lower leg
(reassess limb for distal circulation, sensation and function after securing leg straps) - E – Evaluate traction (ensure that the appropriate amount of traction is still being applied)
- S – Stirrup strap can be "micro-adjusted" to fine tune the exact amount of traction being applied
(reassess limb for distal circulation, sensation and function after adjusting stirrup strap)
Treatment of Open Chest Wounds (Pneumothorax)
.jpg)
Open chest wounds, also commonly referred to as sucking chest wounds, can indicate and contribute to an immediately life-threatening condition known as Tension-Pneumothorax. Essentially, the air normally moved in and out of the patient's lungs during respiration escapes through the ruptured thoracic tissues and accumulate in the thoracic cavity. Atomospheric air may also contribute to this accumulation if air enters into the cavity through the external wounds. The cumulative pressure of air trapped between the chest wall and internal organs can push and squeeze those organs in a manner that prevents their normal function. Most immediately this can affect the patient's ability to breathe and eventually cause cardiac failure.
What the EMALB Examination Guidelines say:
- Cover open chest wounds with a vented occlusive dressing or a commercial chest seal.
Contradictory information in the Emergency Care for Professional Responders text book:
- The Canadian Red Cross Emergency Care text book states that only non-occlusive dressings should be used for treatment of an open chest wound.
What this means for Emergency Medical Responders in BC:
- Emergency Medical Responders in British Columbia will utilize a Vented Occlusive Dressing or Commercial Chest Seal to treat an open chest wound.
- Rescuers should periodically check the Vented Occlusive dressing to ensure that the open end of the valve has not become sealed with drying/sticky blood and therefore become completely occlusive, which will accelerate the tension pneumothorax. If the Vented Occlusive dressing has become sealed, the rescuer should re-open the valve with their finger or similar instrument.
Treatment of Burn Injuries
.jpg)
Burn injuries can continue to cause additional pain and tissue damage even after the source of heat that originally created the burns has been removed. This is partly due to heat from the initial burn becoming trapped in the deep tissue layers surrounding the injured area, and continuing to inflame those tissues. For this reason, it is important to initiate cooling of burn injuries as soon as possible, so long as this does not distract you from dealing with other more crucial priorities. Cooling of burns, most often with sterile saline solution, may be initiated on-scene then continued while enroute to definitive medical care if life-threatening conditions put the patient into the urgent transport category.
What the EMALB Examination Guidelines say:
- Cool any burns 15-20 minutes on scene if patient is stable. Transport and continue cooling enroute if unstable.
- Use pain control measures (e.g. cold, Entonox) if appropriate.
- Applying ice directly to a burn can cause tissue ischemia.
Contradictory information in the Emergency Care for Professional Responders text book:
- The Canadian Red Cross Emergency Care text book states that burns should be cooled at least 10 minutes.
What this means for Emergency Medical Responders in BC:
- Emergency Medical Responders in British Columbia will cool burn injuries for at least 15 minutes, or up to 20 minutes as required.
- Cooling of burns can take place on-scene if there are no urgent/life-threatening circumstances which require immediate tranport.
- Cool, gently running/potable water is the preferred cooling agent.
- In cases where urgent transport is required, burns can be cooled enroute.
- Monitor the patient for early signs of hypothermia when cooling burns which cover a large body surface area (BSA).
- Once cooling efforts have concluded, the wound should be covered and secured with dry, sterile dressings to mitigate the risk of infection. Wet or moist dressings do not provide protection from ambient bacteria.
- Entonox may be considered for pain relief when appropriate.
- Cold packs may be applied for pain relief after initial cooling efforts, provided the patient has unimpaired circulation in the relevant injured extremities.
Assessment of Stroke & TIA
.jpg)
When a blood clot, embolism, plaque or aneurysm prevents adequate blood flow to the brain, a part of the brain tissue can starve or die, causing a stroke. In some cases the blood flow may resume before permanent damage occurs, which is commonly referred to as a Transient Ischemic Attack (TIA). The longer the blood flow is disrupted the more brain tissue dies and the more dramatic and permanent the damage becomes. As the left side of the brain controls the right side of the body, and the right side of the brain controls the left side of the body, the physical effects/deficits created by the stroke are usually seen on the opposite side of the affected brain. Other than early recognition of the signs and symptoms of a potential Stroke, including sudden headache, one-sided weakness/paralysis, dizziness, confusion and slurred speech, there is very little that rescuers can do in the field to prevent ongoing brain tissue ischemia. The sooner a Stroke patient is transported to definitive medical care, the less brain function they will lose and the greater their chances of survival and recovery.
What the EMALB Examination Guidelines say:
- As soon as possible utilize the FAST-VAN pre-hospital stroke tool.
FAST-VAN Pre-Hospital Stroke Tool
- F – Facial droop? (Right-sided or Left-sided)
- A – Arm weakness/paralysis? (Right-sided or Left-sided)
- S – Speech slurred?
- T – Time
Did the symptoms first occur less than 6 hours ago? (< 6hrs)
Or did the patient wake up with the symptoms? - If "yes" to any one of F, A, or S, and to yes to T...proceed with VAN questions
If "yes" to any one of F, A, or S, and to no to T... urgent transport to nearest hospital
(reassess limb for distal circulation, sensation and function after pulling traction) - V – Vision (Right Gaze? or Left Gaze?)
- A – Aphasia? (naming difficulties)
- N – Neglecting/ignoring one side of the body? (typically left side)
- If "yes" to any VAN questions...notify receiving hospital of possible large vessel occlusion
Contradictory information in the Emergency Care for Professional Responders text book:
- The Canadian Red Cross Emergency Care text book includes a different variation of the "FAST" mnemonic for stroke signs and symptoms, but the "T" in time has a different connotation from the EMALB FAST-VAN model. The Emergency Care text book does not include or reference the VAN questions or their corresponding actions.
What this means for Emergency Medical Responders in BC:
- Emergency Medical Responders in British Columbia will utlize the FAST-VAN pre-hospital stroke tool when assessing patients for potential stroke.
- Urgent transport to definitive medical care remains a priority for any suspected stroke patients, regardless of whether or not the VAN questions were included with the on-scene assessment.
- Rescuers should alert inbound hospitals of potential large vessel occlusion as part of ongoing communications when appropriate.
Which Medications Licensed Emergency Medical Responders are Authorized to Administer in BC
.jpg)
The ability to administer medications to patients is a critical part of delivering emergency medical care, and carrys a correspondingly significant set of responsibilities. Licensed Emergency Medical Responders in BC are not authorized to provide all medications in all circumstances, and in many circumstances it is harmful to provide or assist with the wrong medication. Distinguishing between medications which can be administered, medications that can be assisted with, and medications which are contraindicated requires a strong understanding of pharmacology and continuous, ongoing review of current medication guidelines.
What the EMALB Examination Guidelines say:
BCEHS and the EMALB restrict licensed Emergency Medical Responders to Administering only specific medications. As an Emergency Medical Responder holding a BC EMALB License, you are authorized to carry administer the following medications, while employed in your duties as an EMR:
- Oxygen
- Glucogel
- Nitroglycerin
- Acetylsalicylic Acid (ASA)
- Nitrous Oxide (Entonox)
- Naloxone (Narcan)*
*Naloxone administration is not currently included in the baseline scope of practice for a licensed Emergency Medical Responder, but specific emergency response agencies in BC have special permission from BCEHS for their medical responders to carry and administer Naloxone, to mitigate the ongoing opioid overdose crisis. If the agency you work for, in your capacity as a licensed EMR/FR has this agreement in place you will receive agency specific training and then be authorized to carry and administer Naloxone as part of your medical response duties.
What this means for Emergency Medical Responders in BC:
Licensed Emergency Medical Responders in BC will Administer Oxygen, Glucogel, Nitroglycerin, ASA, Entonox and Naloxone* to patients when appropriate and in accordance with the specific protocol, indications and contraindications relevant to that particular medication.
- Any other medications that the patient wants to take which might be acutely beneficial, fall under the general principles of "Assisting" only.
Medication Administration Protocols
- Administration of authorized medications requires that the medical responder ensures that the "Indications" have been met, the "Contraindications" (and relevant "Cautions") have been ruled out, and the protocols for route, doseage and frequency are followed.
- In some cases, administration of a medication may additionally require case-by-case permission from Clini-Call.
- In the event that a patient is carrying their own medication, such as Nitroglycerin Spray or ASA tablets, EMALB Licensed Emergency Medical Responders should still administer the medication carried by the responder, as this affords greater sureity that the medication is of the right type and is not expired/contaminated.
Medication Indications & Contraindications
- Indications are signs/symptoms/medical history which collectively confirm that administration of the specific medication is likely to have a positive effect and acutely improve the patient's condition.
- Contraindications are signs/symptoms/medical history which collectively confirm that administration of the specific medication is likely to have a negative effect and acutely worsen the patient's condition.
- Safe administration of any given medication requires that the Indications have been definitively met, and the corresponding Contraindications have been definitively ruled out.
Medication Cautions
- Cautions are very similar to Contraindications in that they are signs/symptoms/medical history which collectively confirm that administration of the specific medication could possibly have a negative effect and acutely worsen the patient's condition.
- In some cases, an existing Caution may only lead to negative effects if it is an extreme or specific version of the circumstance. One such example is the ASA Caution "Recent Surgery". If the recent surgery was something minor such as a hangnail removal, the anticoagulant effects of ASA are unlikely to cause major bleeding from the residual sutures and ASA can still be safely administered. If, on the other hand, the recent surgery was removal of the pancreas, there is a strong possiblility that the anticoagulant effects of ASA could lead to significant internal bleeding, and ASA should not be administered.
- The presence of Cautions can create "gray areas" surrounding the safe administration of medications and the safest approach may be to treat any given Caution as Contraindication.
Vital Signs Prior to Administration
- BC EMALB practical examination guidlines for Emergency Medical Responders stipulate that a complete set of "baseline" Vital Signs must be assessed and documented prior to administration of medications.
- A full set of Vital Signs collected before administering a medication will aid in assessing any positive or negative effects the medication has on the patient.
- Administration of Acetylsalicylic Acid (ASA) is the only exception to this requirement.
Assisting with Medications
- In the event that a patient requires a medication that they have on hand, and for which an Emergency Medical Responder is not authorized to administer, it may be appropriate for the EMR to "Assist" the patient with that medication.
- It is important to be clear on the differences between Assisting with and Administration of medications from an EMALB Licensing standpoint.
- Administration of a medication involves the medical responder making all decisions regarding the necessity, dose, and freqency of the medication (as well as carrying the medication itself).
- Assisting with medication, on the other hand, requires that the patient themselves has made all the decisions, and has followed through on all the required actions involved with self-administering their medication.
- The EMALB Licensed medical responder's role in "Assisting" with medication could include retreiving the medication from a nearby location (such as from the patient's bedroom or bathroom), as well as opening and/or preparing the medication for use. However, it should be the patient themselves who actually self-administers the medication.
- If, for example, an EMALB Licensed medical responder retrieves an EPI-Pen which the patient has requested from the other room and hands it to the patient, that constitutes Assisting, which is within the scope of licensure and therefore permissable.
- If, on the other hand, an EMALB Licensed medical responder injects the EPI-Pen into the patient's thigh for them, this could be considered Administration of Epinephrine, which is outside the scope of licensure. Such action would put the medical responder in an ethically precarious position, and potentially leave them open to legal repercussions.
- The line between Assisting and Administering medications can become blurry, and the safest option may to be refrain from Assisting.
- Prior to Assisting with medication, a best practice is to review the "6 Rights" of medication to ensure that the chances of harm are minimized. In many cases, it may also be advisable to consult CliniCall/medical oversight prior to Assisting with any particular medication.
6 "Rights" of Medication
The 6 Rights of Medication are a memonic device to aid medical responders in systematically ensuring that assisting a patient with their medication is likely to be beneficial and unlikely to be harmful. If an EMALB Licensed medical responder is going to actually "Administer" medication, the specific protocols, indications, contraindications and cautions should be followed rather than the 6 Rights.
- P – Right PERSON
Is this the person's own medication, and/or has it been prescribed to them by a doctor? - M – Right MEDICATION
Is this the medication the patient intends to self-administer, and/or is this particular medication likely to be acutely beneficial and improve the patient's condition? - T – Right TIME
Has the the time of self-administration been documented and/or has an appropriate amount of time elapsed between doses? - D – Right DOSE
Is the proper amount of medication of being self-administered? - R – Right ROUTE
Is the proper method of self-administration being followed? - D – Right DOCUMENTATION
Has the name of the medication, dose taken, route of self-administration, time of self-administration and/or any positive or negative effects been documented?
EMALB Licensed Emergency Medical Responders may routinely utilize the 6 Rights mnemonic to Assist patients with (but not Administer) commonly prescribed medications which can have acutely beneficial effects such as an EPI-Pen which delivers Epinephrine, and Asthma Inhalers which deliver Salbutamol/Albutrol.
Glucogel for Unresponsive Patients
.jpg)
For patients with confirmed Hypoglycemia, which in BC is considered a measured capillary blood glucose level (capBgl) below 4 mmoL/l, quickly raising their blood sugar levels can alleviate immediately life-threatening conditions including the associated decreased levels of consciousness. Glucose Gel (Glucogel) can be administered orally and alleviate hypoglycemia with little risk of negative effects or drug interactions, however there is a risk that the patient may choke on the gel if they are not completely responsive at the time of administration.
What the EMALB Examination Guidelines say:
- Glucogel can only be administered to Patients who are responsive enough to obey commands.
Contradictory information in the Emergency Care for Professional Responders text book:
- The Canadian Red Cross Emergency Care text book outlines the procedure for administering Glucogel to an unresponsive patient, but does stipulate that this is only to done where local protocol permits.
What this means for Emergency Medical Responders in BC:
- Unresponsive patients who cannot obey commands will not receive Glucogel or any orally administered glucose.
- Patients with a confirmed blood glucose level (CapBgl) of less than 4 millimoles/liter (mmol/L), but are still able to obey commands, should be administered 12-15 grams of Glucogel prior to transport.
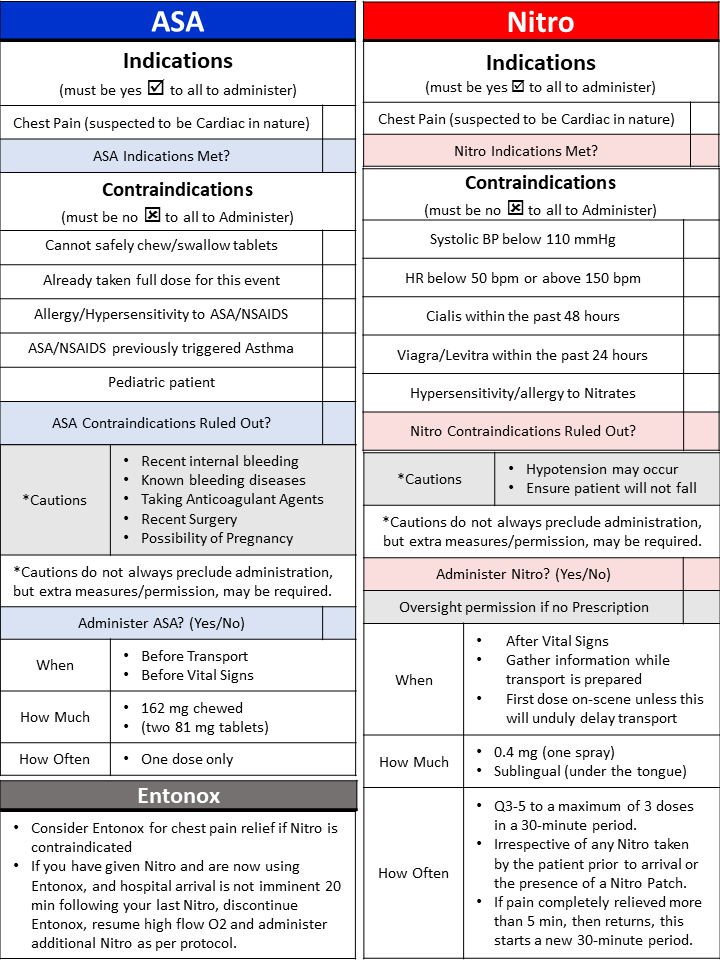
Administration of Nitroglycerin to Patients with or without a Prescription
.jpg)
Nitroglycerin spray is a vasodilator, which means that the correct dose at the correct time can temporarily and partially alleviate the symptoms of acute myocardial infarction (AMI). The vasodilation that accompanies a dose of nitro can widen coronary arteries and leave more room for blood to flow past a blockage. Nitroglycerin can also create a dramatic drop in blood pressure, which can itself cause negative patient outcomes if not carefully monitored and mitigated. Administration of Nitro spray, whether to a patient with a previous Nitro prescription or to a patient with no previous prescription, requires strong familiarity with and stringent adherence to the associated protocols surrounding indications, contraindications, cautions, doeseage and frequency.
What the EMALB Examination Guidelines say:
Nitro Indications
- Patients whose presentation is suggestive of cardiac chest pain, who have a history of heart disease, and who would normally take their prescribed Nitroglycerin for chest pain.
- Systolic Blood Pressure above 110 mmHg
- Heart Rate above 50 bpm and below 150 bpm (Non-prescribed only)
- Clin-Call Permission (Non-prescribed only)
Nitro Contraindications
- Known allergy or sensitivity to Nitrates
- Patient has used Viagra or Levitra in the past 24 hours
- Patient has used Cialis in the last 48 hours
Nitro Protocol
- Hypotension frequently occurs, especially in the elderly and must be expected. Ensure patient is not at risk to fall.
- If your patient has a Nitro patch applied, it does not change the Nitroglycerin protocol.
- If patient is not on Nitroglycerin, systolic pressure >100; HR >50 and <150 Nitroglycerin may be administered after mandatory consultation with medical oversight.
- Patient outcome is better if definitive hospital treatment is provided as soon as possible, hence early transport is highly desirable. When equipment is ready load and transport, do not delay until after the first Nitroglycerin if everything else is ready to go; load and go and treat en route.
- Ensure that Systolic Blood Pressure is above 110mmHg and check whether pain still persists before administrating repeat Nitroglycerin. Contact medical oversight if needing to go beyond 3 doses or if patient condition changes.
- Repeat vitals and drug until pain is relieved, to a maximum of 3 doses in any 30-minute period (providing the systolic BP remains above 110; irrespective of any Nitro taken by the patient prior to your arrival).
- If pain is completely relieved for more than 5 min, you may initiate the chest pain protocol again if the pain returns. This is considered a new episode which starts a new 30-minute period. This is applicable even if Nitro has already been administered for the initial episode.
Contradictory information in the Emergency Care for Professional Responders text book:
- The Emergency Care text book states that a Systolic Blood Pressure of less than 100 mmHg contraindicates the administration of Nitroglycerin.
- The Emergency Care text book also stipulates that Nitroglycerin can only be administered once every 5 minutes, to a maximum of 3 doses, but does not outline parameters for starting a "new" 30-minute time period.
What this means for Emergency Medical Responders in BC:
- Nitroglycerin should be considered when the Indications have been met and the Contraindications have been ruled out.
- Nitroglycerin can be administered to a patient without a prior prescription if their Systolic blood pressure is above 100 mmHg and their heart rate is between 50 – 150 beats per minute.
- CliniCall must be consulted before administering Nitroglycerin to a patient without a prior prescription. (1-833-829-4099)
- The first dose of Nitroglycerin should ideally be administered after placing the patient on the cot, but before initiating transport.
- However transport should not be significantly delayed just to administer Nitro, and treatment enroute is considered effective.
- Nitroglycerin can be administered in 0.4 mg doses (1 sublingual spray) every 3 minutes (q3), provided the Indications continue to be met, and the Contraindications continue to be ruled out.
- CliniCall must be consulted before administering a 4th (or more) dose of Nitroglycerin to any patient, regardless of whether or not they have prior prescription. (1-833-829-4099)
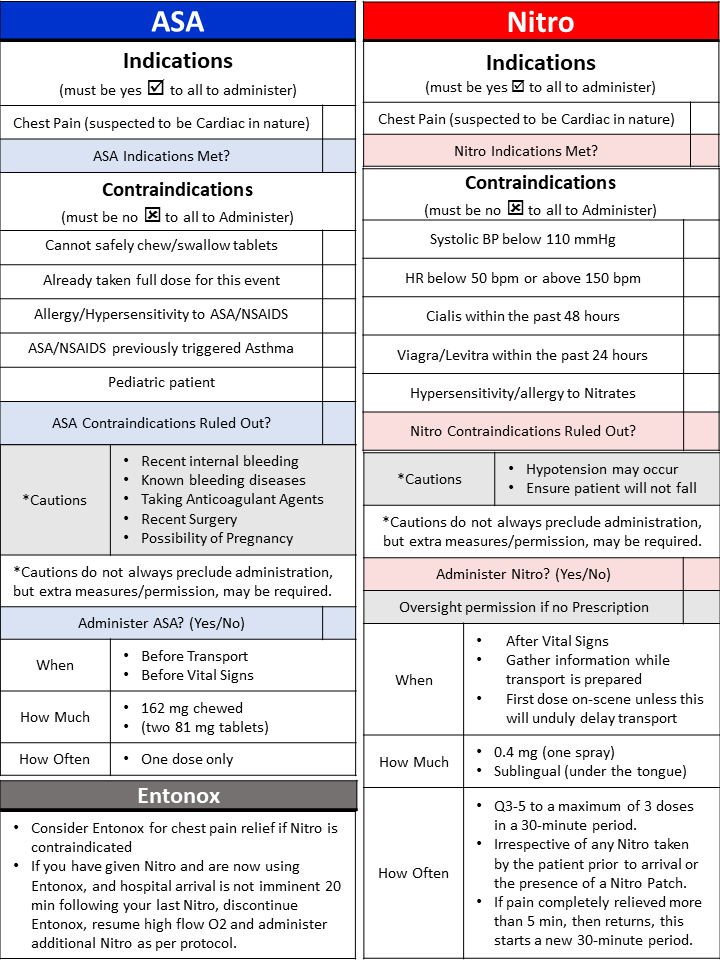
Administration of Acetylsalicylic Acid (ASA) before Vital Signs
.jpg)
Acetylsalicylic Acid (ASA), also commonly referred to as Aspirin is both a platelet inhibitor and an anti-inflammatory. These properties can make ASA an extremely important and effective medication for patients experiencing acute myocardial infarction (AMI), as the platelet inhibitor effects prevent blood clots in the corornary artery from growing larger and the anti-inflammatory effects prevent the walls of the coronary ateries from becoming swollen and closing in on existing blockages. Because the positive effects of ASA during an AMI are so pronounced and time sensitive, it is the only only medication which can be administered without first collecting a complete set of Vital Signs.
What the EMALB Examination Guidelines say:
ASA Indications
- Chest pain or atypical symptoms consistent with cardiac ischemia/acute myocardial infarction (AMI).
ASA Contraindications
- Known hypersensitivity or allergy to ASA or other (NSAIDS) agents.
- Patients with a history of asthma induced by the administration of salicylates or NSAIDS.
- Pediatric patients with viral symptoms
ASA Cautions
- Recent internal bleeding
- Known bleeding diseases
- Patient is currently taking anticoagulant agents
- Recent surgery
- Possibility of pregnancy
ASA Protocol
- 160 mg of ASA should be given orally, after RBS and before vitals as long as it is indicated and the cautions and contraindication are followed
What this means for Emergency Medical Responders in BC:
- When a patient is showing Signs and Symptoms suggestive of a possible heart attack, Responders should immediately utilize the SAMPLE-OPQRST mnemonics (History) to determine if ASA is appropriate.
- If appropriate, have the patient chew two 81mg ASA or one 325 mg ASA before initiating transport or assessing the Vital Signs.
- ASA is the only medication which does not require a full set of Vital Signs before Administration
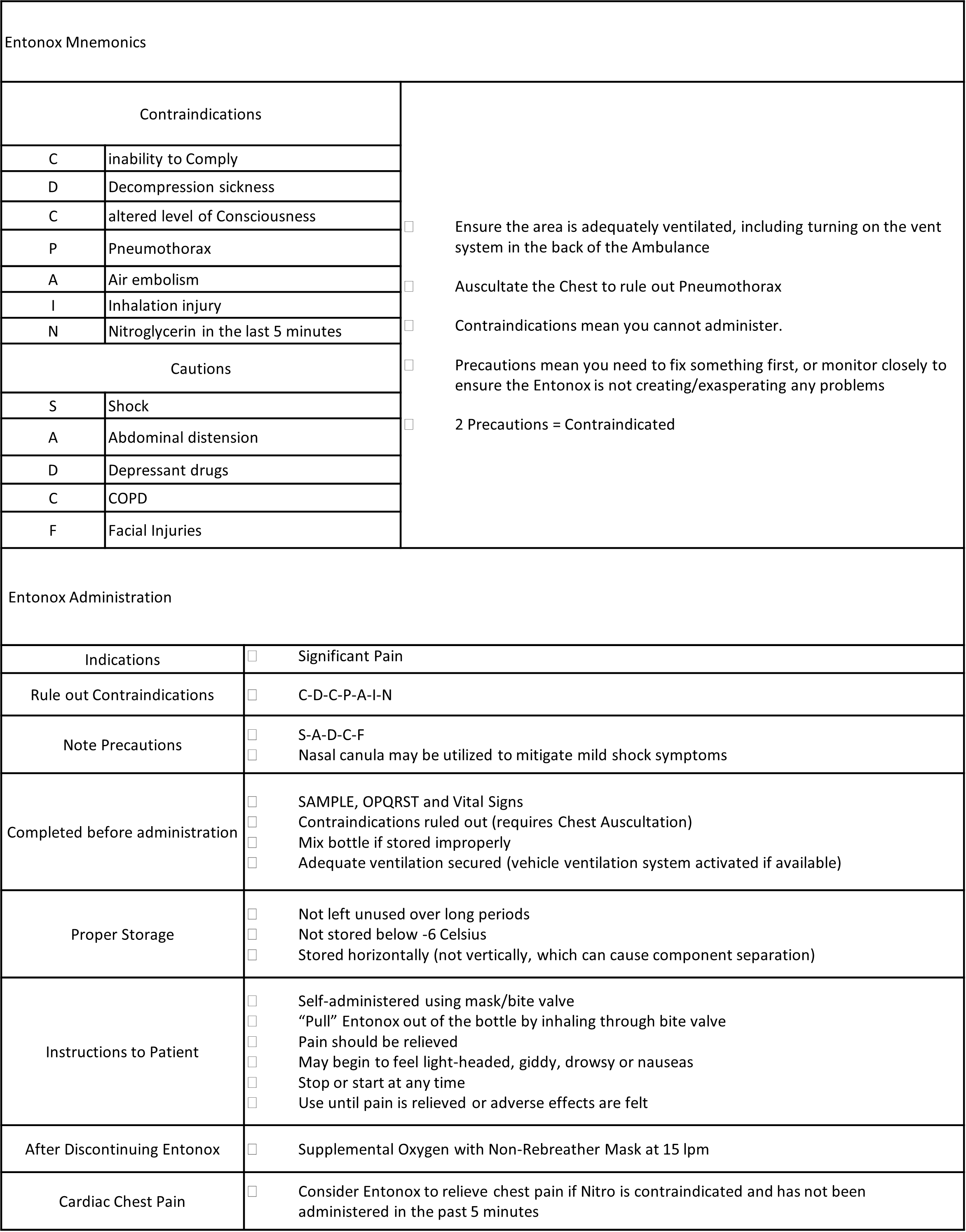
Administration of Nitrous Oxide (Entonox)
.jpg)
Nitrous Oxide (Entonox), also commonly referred to as laughing gas, is a fast acting analgesic gas which can be self-administered by patients under the guideance and supervision of a Licensed Emergency Medical Responder in BC. Entonox is indicated, and should be considered, for any patient experiencing significant pain or physical discomfort, however the corresponding gases that permeate the lungs and bloodstream can cause significantly negative patient outcomes if contraindicated. Most often, Entonox is provided to patients with a simple, non-life-threatening femur fracture as part of applying a Sager Traction Splint. Entonox is also appropriate for patients experiencing cardiac chest pains if Nitroglycerin is contraindicated or not available.
What the EMALB Examination Guidelines say:
Entonox Indications
- Pain
Entonox Contraindications
- C – inability to COMPLY
- D – DECOMPRESSION sickness
- C – altered level of CONSCIOUSNESS
- P – PNEUMOTHORAX
- A – AIR emboli
- I – INHALATION injury (Entonox may be administered to patients with suspected inhalation injuries if O2 saturation is 100%.)
- N – NITROGLYCERIN use within 5 minutes
Entonox Cautions
- S – SHOCK
- A – ABDOMINAL distenstion
- D – DEPRESSANT drugs
- C – COPD
- F – FACIAL injuries
Entonox Protocol
- Complete a primary survey.
- Conduct a history and physical examination sufficient to rule out the contraindications for use of Entonox (S-A-M-P-L-E).
- Investigate the pain complaint, including severity (O-P-Q-R-S-T).
- Obtain a baseline set of vital signs, including oxygen saturation.
- Invert the Entonox cylinder 3 times to ensure the gases are properly mixed.
- Ensure adequate ventilation (if in the ambulance, turn on vehicle ventilation system).
- Provide patient with instructions on self-administration.
- Instructions should include a list of possible side-effects (light-headedness, dizziness, sedation, drowsiness, disorientation, nausea and/or vomiting).
- Let patient use bite stick or apply mask to own face, do not assist.
- Mask/bite stick may fall away as patient becomes sedated, do not replace mask.
- Patients should receive high-flow oxygen when Entonox is discontinued.
- Discontinue immediately if cyanosis develops.
What this means for Emergency Medical Responders in BC:
- Consider the administration of Entonox for relief of moderate to severe pain.
- This includes cardiac related chest pain where nitroglycerin will be of no value or is contraindicated
- Commonly administered for isolated extremity injuries, and pain associated with burns.
- Administration of Entonox should not delay initiation of urgent transport if there are life-threatening considerations.
Administration of Naloxone (Narcan) to Reverse Opioid Overdose
.jpg)
Administering Narcan, in either intramuscular or intrnasal form can temporarily alleviate the most life-threatening aspects of Opioid overdose, such as respiratory arrest and unresponsiveness, but it does not completely remove the poison from the person's system. The opioids will remain in the system after the Naloxone has dissipated, so it is vital that someone receives definitive clinical medical care as soon as possible following the overdose and subsequent Narcan administration. The administration of Naloxone, once appropriate, may further support these critical interventions by increasing the patient's level of conciousness and/or improving their natural respiration rate, rhythm and character. Although multiple doses of Naloxone, at increasing dosages, may be required for optimal patient care, it is not necessary to completely reverse all the effects of the opoiod or achieve full patient responsiveness, as long as the airway remains clear and adequate respirations resume.
What the EMALB Examination Guidelines say:
Naloxone (Narcan) is a narcotic antagonist which antagonizes opioid effects by competing for the same receptor sites. This antagonistic action reverses the effects of opioids including respiratory depression, sedation, and hypotension.
Naloxone Indications
- To reverse respiratory depression/depressed mental status secondary to actual or suspected narcotic use.
- Decreased LOC in a patient with a history that suggests narcotic overdose
- Difficulty in maintaining the patient’s airway
- Respiratory rate <10 per minute
Naloxone Contraindications
- Allergy or known hypersensitivity to Naloxone
- Neonatal Patient
Naloxone Cautions
- Patient combativeness.
- May precipitate withdrawal symptoms.
Prior to Naloxone Administration
- Primary airway management is paramount by ensuring the patient’s airway is protected, open and clear.
- Ensure the patient is well oxygenated and/or ventilated with a BVM.
- Complete the Primary survey.
- Confirm a history sufficient to suggest narcotic overdose as the cause of unconsciousness.
- Obtain a history sufficient to rule out contraindications for the suspected narcotic overdose protocol.
- Obtain a complete baseline set of vitals.
First Naloxone Dose
- Administer 0.4 mg Naloxone Hydrochloride through intramuscular injection (IM)
- Load and transport immediately following first dose.
- Provide additional doses every 3 minutes (q3) as required if there is no improvement in the patient's condition.
Second Naloxone Dose
- If no improvement 3 minutes after the first dose, administer 0.4 mg Naloxone Hydrochloride through intramuscular injection (IM)
- Provide additional doses every 3 minutes (q3) as required if there is no improvement in the patient's condition.
Third Naloxone Dose
- If no improvement 3 minutes after the second dose, administer 0.8 mg Naloxone Hydrochloride through intramuscular injection (IM)
- Provide additional doses every 3 minutes (q3) as required if there is no improvement in the patient's condition.
Fourth Naloxone Dose
- If no improvement 3 minutes after the third dose, administer 2.0 mg Naloxone Hydrochloride through intramuscular injection (IM)
- Also consider assessing blood glucose level.
- If blood glucose ≤ 4mmol/L, consider diabetic protocol.
Contradictory information in the BC Emergency Health Services Act:
- Administration of Naloxone is not specifically outlined in either Schedule 1 or Schedule 2 of the BC Emergency Health Services Act, which defines the scope of practice for an EMALB Licensed Emergency Medical Responder.
What this means for Emergency Medical Responders in BC:
- Some specific, individual emergency response agencies throughout BC, including ambulance services and many Fire/Rescue Departments, have entered into an agreement with BCEHS to provide Naloxone through a special agreement. This is essentially "special permission" to carry and administer Naloxone when responding to 9-1-1 medical incidents.
- If the agency you work for, as a medical responder, has such an agreement in place with BCEHS, you will receive additional training from that agency with regard to Naloxone administration. However, it is important to note that this special permission can be withdrawn at any time, and is only applicable when providing emergency medical services for that specific agency.
- Naloxone administration is not technically included within the scope of your EMALB Licence.
- Naloxone should be considered when responding to a medical incident where opioid overdose is either suspected or confirmed.
- The decision to administer Naloxone will be based on several factors including surroundings, bystander accounts, presence of drug paraphernalia, and patient signs and symptoms.
- When present simultaneously, depressed or absent respirations, decreased level of consciousness, and pinpoint pupils are considered the "Palindrome" of opioid overdose. These three signs and symptoms should be collectively considered a strong indication of opioid overdose.
- Follow the EMALB Examination Guidelines protocol for Naloxone administration (outlined above) when appropriate.
- CliniCall must be consulted before administering more than 4 doses of Naloxone. (1-833-829-4099)
- The goal of Naloxone administration is to reverse respiratory depression so that the patient begins to breathe effectively on their own.
- It is not necessary to restore full levels of consciousness through administration of Naloxone, and doing so may result in combative behaviour.
Examination Guidelines Contents:
- Scope of Practice (services & endorsements)
- Patient Assessment Model
- Patient Assessment Model - Guidelines
- Patient Assessment Model - Primary/Survey Assessment Interventions
- Critical History Questions
- Assessing LOC Using AVPU
- Glasgow Coma Scale
- Abbreviations
- Patient Care Report
- References
- Wound Care
- Preservation of Amputated Parts
- Fracture Management
- Fracture Management - Traction Splint
- Spinal Management
- Burn Management
- Hypothermia
- CVA - Stroke - Flowchart
- Abdominal Injuries - Flowchart
- Chest Trauma - Flowchart
- Electrical Contact - Flowchart
- Heat Exhaustion/Heatstroke - Flowchart
- Drowning/Near Drowning - Flowchart
- IV Procedures
- IV Maintencance
- IV Maintenance Rate Calculation
- Adult CPR/AED
- Child Infant CPR/AED
- Foreign Body Airway Obstruction
- Cardiac Chest Pain PCP/EMR
- Nausea - Vomiting PCP
- Shortness of Breath (SOB) With History of Asthma/COPD - PCP
- Oxygenation Management - Pulse Oximeter PCP/EMR
- Continuous Positive Airway Pressure (CPAP) PCP
- Entonox PCP/EMR
- Hypovolemia - PCP
- Anaphylaxis - PCP
- Unconscious Not Yet Diagnosed (NYD) - PCP
- Suspected Narcotic Overdose - PCP/EMR
- Diabetic Emergencies - EMR
- Diabetic Emergencies - PCP
- Aspirin (ASA)
- D10W (Dextrose 10% in Water)
- Dimenhydrinate
- Diphenhydramine
- Entonox (Nitrous Oxide)
- Epinephrine
- Glucagon
- Naloxone (Narcan)
- Nitroglycerin
- Oral Glucose
- Salbutamol (Ventolin)
- Tranexamic Acid
EMA Licensing Board Examinations
- Practical Examination Grading Criteria
- Star Weighting
- Practical Exam Appeals
- Exam Reviews
- EMR Examination Requirements
- Scheduling EMR Examinations
- PCP Examination Requirements
- Scheduling PCP Examinations
- Licence Fees
- How to Pay Your Licence Fees
- Licence Applications
EMA Licensing Board Examination Policies
- EMALB 2011-01 Candidate Code of Conduct
- EMALB 2012-02 Failure to Attend or Late Notice of Cancellation
- Change Index
tel: 778-724-9054 email: training@mediprofirstaid.com
We recognize and respectfully acknowledge that we operate on the traditional and unceded territory of the Syilx Okanagan and Secwepemc peoples.

.png)
.png)