Wilderness First Responder
Wilderness First Responder Course Summary
| WFR Course Registration |
| WFR Course Overview |
| WFR Course Preparation |
| WFR Course Skills |
Wilderness First Responder training gives you the skills and knowledge you need to be a leader during a medical emergency in a recreational or professionally guided outdoor setting. Learn how to treat injuries and illnesses in remote areas of the wilderness using the supplies available, and make critical decisions about emergency transport, improvised shelters, communications and group safety. You'll learn and practice a systematic and flexible approach to manage a wide range of outdoor emergencies in variable circumstances. This includes decisions and actions surrounding CPR & AED, Choking, Deadly Bleeding, Heart Attack, Stroke, Wound Care, Splinting, Diabetes, Concussion, Spinal Injuries, Hypothermia, Heat Stroke, Poisoning, Overdose, Shelter Options, and Remote Transport.
Advanced first aid skills combined with clinical decision making and outdoor leadership will help prepare you for your next guiding, camping or paddling adventure. A strong emphasis on developing a safety first attitude will help you anticipate and prevent many common injuries before they even occur. Responding to emergencies following a logical and consistent decision making process is the underlying foundation of your Wilderness First Responder training. Rather than being forced to memorize a rigid and outdated list of "rules" you'll practice a simple yet flexible approach to making sound decisions and taking sensible action that gives you confidence in any situation, regardless of the nature and extent of the injuries. You'll acquire the skills and confidence to Be the Difference when it matters.
Wilderness First Responder Certification
Upon successful completion of the Wilderness First Responder program you will recieve an WFR certificate, as issued through the Canadian Red Cross, valid for 3 years. You will also receive a separate Basic Life Support (BLS) certificate valid for 1 year. Canadian Red Cross certificates are generated and issued electronically through the national MyRC database, and provided by email within 10 business days of completion of all course and examination requirements. More...
Basic Life Support (BLS) Certification
Upon successful completion of the Wilderness First Responder program you will recieve a Canadian Red Cross BLS certificate, as issued through the Canadian Red Cross, valid for 1 year. Basic Life Support course content includes CPR-AED skills for adult, child, infant and neonatal patients, multi-Rescuer dynamic CPR performance, variable compression to ventilation ratios, airway management, and oxygen therapy. More...
Course Duration & Recertification
Wilderness First Responder courses are typically delivered over 8-10 consecutive classroom sessions. If you already hold a current, valid and un-expired Wilderness First Responder certificate, you are eligible to participate in a shortened WFR Recertification course. There is also an online based Wilderness First Responder study guide, which participants are encouraged to complete prior to or during the WFR course itself. Study Guide completion time will vary with each participant's individual study habits, learning style and schedule. However you should anticipate approximately 8-12 hours of independent, self-directed time to complete the Study Guide. More...
Wilderness First Responder Course Overview
Review the information in this section to make sure that Wilderness First Responder will meet your training and certification needs, and give yourself the tools to arrive fully prepared for success and enjoyment in your WFR course. Wilderness First Responder certification training, and the corresponding BC EMALB Licensing process require a significant investment of time and effort, so you should make sure you know what you're getting, and what you're getting into.
What You Get
.jpg)
What's included with your Kelowna Canadian Red Cross Wilderness First Responder course and registration fees?
- Canadian Red Cross Wilderness First Responder (WFR) certification (valid for 3 years).
- Canadian Red Cross Basic Life Support (BLS) certification (valid for 1 year).
- Canadian Red Cross Wilderness & Remote First Aid Field Guide (online access to the PDF version is included with your registration and you have the option to purchase a printed take-home copy)
- Canadian Red Cross Emergency Care for Professional Responders reference manual (online access to the PDF version is included with your registration and you have the option to purchase a printed take-home copy).
- Online Wilderness First Responder Study Guide.
- Access to Medi-Pro's extensive library of online resources and support materials.
Canadian Red Cross WFR Certification
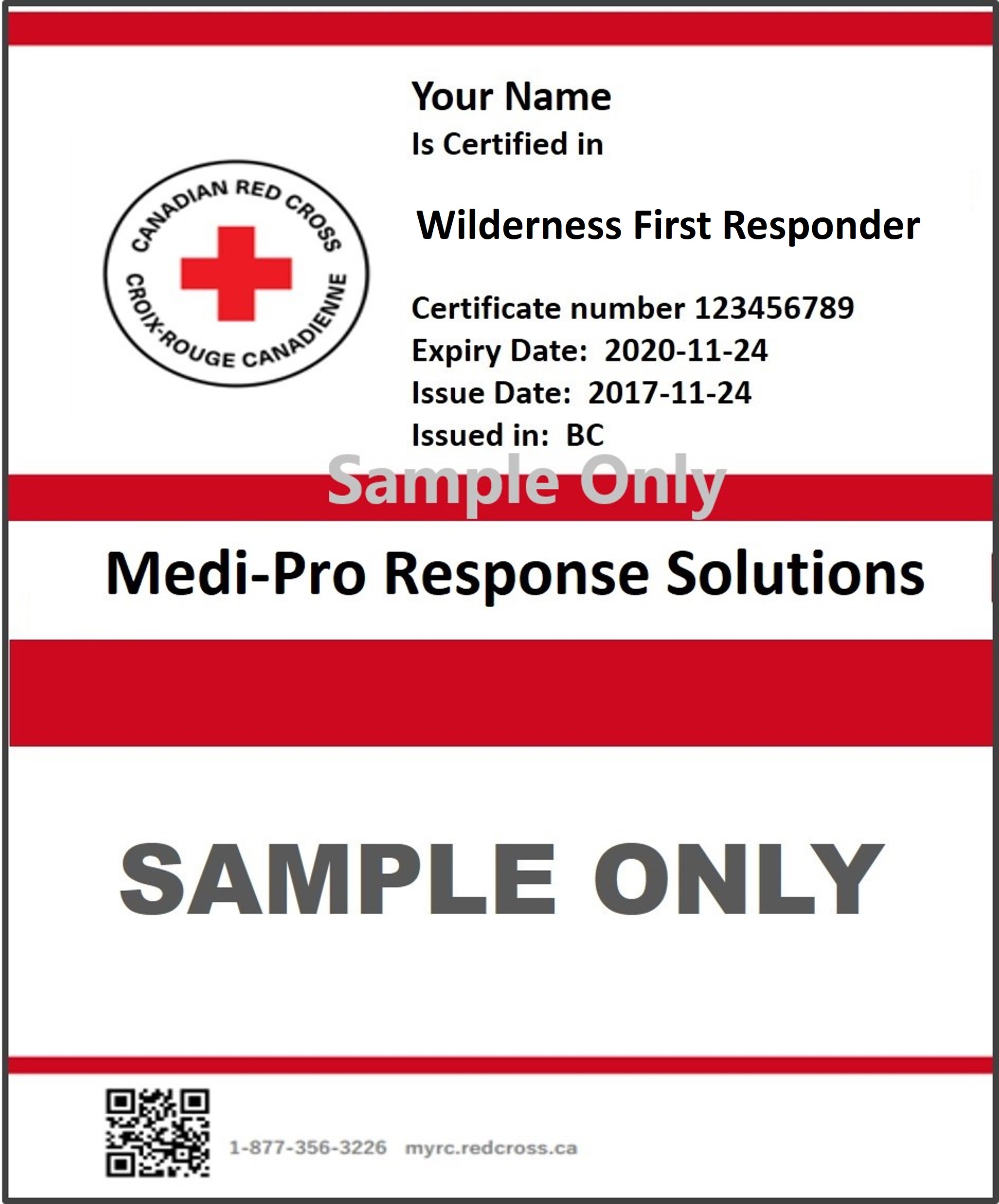
Our Canadian Red Cross Wilderness First Responder programs are Nationally recognized for up to date protocols, and meet the most current BCEHS Clinical Practice Guidelines, and BC EMALB Licensing requirements.
You'll learn and practice advanced emergency medical assessment and interventions which will help you make safe decisions in any emergency, and provide professional medical care to your patients.
Your Canadian Red Cross WFR certificate, awarded to you upon completion of your Kelowna WFR course and valid for 3 years, will indicate Canadian Red Cross Wilderness First Responder certification. You will also receive a Canadian Red Cross Basic Life Support (BLS) certificate, valid for one year.
Canadian Red Cross certificates are generated and issued electronically through the national MyRC database, and provided by email within 10 business days of completion of all course and examination requirements. More than just a certificate, you'll have the confidence to act, and Be the Difference in your community.
Basic Life Support
.png)
In addition to your 3 year Wilderness First Responder (WFR) certificate, you will also receive a separate Basic Life Support (BLS) certificate which is valid for 1 year. Basic Life Support is essentially a high performance, "pit-crew" approach to Cardiopulmonary Resuscitation (CPR) and Automated External Defibrillation (AED) in a professional medical responder environment.
Basic Life Support principles form an integral part of your overall Wilderness First Responder training, and are also considered a standalone, portable skill set that can be transferred to work with any high performance team performing CPR in a clinical setting. Your Wilderness First Responder certification includes BLS protocols, and remains valid for 3 years, however the separate Basic Life Support certificate issued at the same time will only remain valid for 1 year. If you require a valid BLS certificate, you will need to complete a standalone BLS Recertification course yearly, but your WFR certificate will remain valid for the full 3 year term regardless of whether or not you specifically renew the BLS certificate.
There is an emphasis on the specific Basic Life Support protocols stipulated and outlined by the local authorities having jurisdiction (AHJ) in British Columbia including the Emergency Medical Assistant's Licensing Branch (EMALB) examination guidelines, BC Emergency Health Services (BCEHS) Clinical Practice Guidelines, and BC Ambulance Service (BCAS) response guidelines. Basic Life Support skills, tools and principles covered in your Wilderness First Responder course include...
- Team based approach to CPR & AED with multiple rescuers/agencies on scene
- Variable Compression to Ventilation ratios for patients in different age groups
- Adult patients aged 9 and up (30:2/10:1/CCC)
- Child patients aged 1 to 9 (15:2)
- Infant patients under 1 year old (15:2)
- Neonatal patients under 28 days old (3:1)
- Bag-Valve-Mask (BVM)
- Oxygen Therapy
- Oropharyngeal Airways
- Nasopharyngeal Airways
- Automated External Defibrillators
- CPR in Transport/Treatable CPR
Where to go
.png)
Our Canadian Red Cross Wilderness First Responder courses are provided in multiple classroom locations in Kelowna, Vancouver, the Lower Mainland and throughout British Columbia. Most WFR courses in the Okanagan area are conducted in our West Kelowna classroom at 2011 Daimler Drive. Click here for directions, maps and public transit options.
By request, we can schedule private courses for your group at specific location of your choosing. The location and directions for your particular Wilderness First Responder course will be indicated during the booking process, and included in the confirmation email you will receive upon completing registration.
- Make sure the WFR course you are registering for is in a location that works for you.
- Our booking platform may show WFR courses at different geographic regions on different course dates.
- Check your confirmation email to ensure that the course location indicated is in the region you expected.
- The link in your confirmation email will incude directions, but you should verify your intended route of travel ahead of time.
- Allow ample time for traffic and unanticipated delays to ensure you arrive at your classroom in time for your scheduled course sessions.
WFR Course Schedule
.jpg)
Get the most out of your Kelowna Wilderness First Responder course by familiarizing yourself with the Wilderness First Responder course content, schedule, and classroom session structure. Your Canadian Red Cross WFR course in Kelowna or Vancouver, BC,, is structured into ten 10-hour classes starting at 8 a.m. each morning. WFR concepts, principles, and skills are introduced in a simplified context and logical sequence. The Wilderness First Responder course starts with basic drills, and builds towards more complex scenarios with an emphasis on clinical decision making as participant skill levels and confidence improve. Stand-alone skill components are introduced and reinforced, then integrated into realistic situations and circumstances. Intensity, workload and student responsibilities increase as the WFR course progresses, with developing emphasis on clinical decision making abilities and adaptive skill application.
Each WFR course session includes two short breaks and one longer lunch break throughout the day. Access to locals stores or restaurants may be limited, so you should arrive at each session with enough food and water/drinks to keep you nourished and hydrated the entire day. The daily course outline listed below is an estimated broad-strokes timeline for the WFR skills, principles and topics and subject to change according to classroom logistics, participant needs and instructional necessity. Your Canadian Red Cross WFR written exam, and two WFR practical scenario evaluations will take place throughout the final classroom sessions.
The closing sessions of your Wilderness First Responder course will focus on reviewing, practicing, and expanding on all the topics, skills and principles covered in previous the sessions. Performing a skill or reading a text passage once will not prepare you for success. In order to be successful in your final evaluations, and in providing patient care as a professional wilderness responder you need to have a reflexive familiarity, born of repetition and feedback, with all aspects of your WFR training. The more you review the key concepts and practice the foundational skills, the more you can focus on problem solving the unique challenges of each patient and circumstance.
These final WFR course sessions will be your opportunity to identify areas that you feel less comfortable with, and ask your Instructor to work with you on them to improve your confidence and skill levels. Most of the time spent in the classroom at this point will be dedicated to full simulation scenarios, and you can request specific topics or versions of these scenarios based on your own evaluation of your readiness and needs as a learner. You may feel comfortable performing CPR as a hands-on skill, but need more clarification on the criteria for Treatable CPR and CPR in Transport. You may have the NEXUS SMR decision matrix memorized, but want to practice the hands-on application of a spinal collar. You will also have the opportunity to practice established skills in more complex scenarios and challenging circumstances to more accurately reflect real-life applications. WFR principles, skills and concepts reviewed, practiced and reinforced throughout the review and practice sessions of your Canadian Red Cross Wilderness First Responder course include...
- WFR Assessment Model review
- Glasgow Coma Scale review
- NEXUS Spinal Motion Restriction criteria review
- FAST VAN Stroke Assessment review
- Manual SMR stabilization practice
- Naloxone (Narcan) Inidications and Contraindications review
- Glucogel Indications and Contraindications review
- Respiratory Distress management practice
- Respiratory Arrest management practice
- Verbal and written patient care hand-over practice
- Pit Crew CPR-AED review
- CPR with Airway Obstruction review
- Review & Practice Medical and Trauma based scenarios
Frequently Asked Questions
.jpg)
Frequently Asked Questions about Canadian Red Cross Wilderness First Responder certification courses in Kelowna and Vancouver BC. Take a look through the Q & A topics listed below, to find answers to your Wilderness First Responder course questions. If you don't see the answers to your questions in this FAQ section, you may still find the information you're looking for in the other sections of this page, including Wilderness First Responder Overview, Wilderness First Responder Resources, and Wilderness First Responder Course Skills.
Of course, Medi-Pro First Aid is happy to answer all your questions if you choose to contact us directly through our Contact Us form, by email (training@mediprofirstaid.com), or over the phone (778-724-9054). We do our best to respond to all enquiries as quickly as possible during normal business hours from 9am to 5pm, Monday-Friday.
Q. When will I get my WFR Certificate?
Canadian Red Cross Wilderness First Responder certificates are generated on the national MyRC course management platform and provided to Wilderness First Responder course participants electronically, in PDF format. Upon successful completion of your Wilderness First Responder course, Medi-Pro will upload and process your certification, and you will recieve your WFR certificate by email. Medi-Pro administration do their best to ensure this process is generally completed within 48 hours of course completion, but it in some circumstances it can take up to 10 business days. If you require immediate proof of Wilderness First Responder course completion, your Instructor can provide you with a temporary certificate before you leave the classroom. However it is up to each individual employer/regulatory agency to decide whether or not they accept temporary certificates. It is usually simplest to just forward your official Wilderness First Responder certificate and/or your Basic Life Support certificate as soon as you receive it.
Q. Can I get a refund if I cancel my Wilderness First Responder course registration?
Medi-Pro's baseline policy is no refunds for last minute cancellations. However, we will do our best to work with you if circumstances beyond your control make it impossible for you to attend your scheduled course. In most cases, we can find an alternative course date for you and just move your existing registration to the new date. Depending on circumstances, and the number of previous cancellations, there may be a small re-booking charge, but we're compassionate people who understand that life can be messy.
Q. How long is an Wilderness First Responder course?
In British Columbia, the minimum classroom time required for a Canadian Red Cross Wilderness First Responder course is 80-100 hours. Medi-Pro generally schedules Wilderness First Responder courses over ten 10-hour days, building an additional 20 hours into your training over and above the minimum requirement. This additional time plays a crucial role in allowing you enough time to not only learn WFR principles for the first time but also perform multiple repetitions of the skills and scenarios and build lasting confidence and leave you prepared for success in your final exams. If your group requires a different timeframe, such as multiple weekends or a specific day of the week broken up across multiple weeks, you can make arrangements with Medi-Pro for a private booking that works for your group's scheduling needs.
Q. Is there an age requirement for Wilderness First Responder courses?
The minimum age to be eligible to receive Canadian Red Cross Wilderness First Responder certification is 16. This means you must be at least 16 years old at the time of course completion, in order to receive a Canadian Red Cross Wilderness First Responder certificate.
Q. Can I renew/recertify my old Wilderness First Responder certificate?
If you hold a current and valid Wilderness First Responder certificate from Canadian Red Cross, St. John Ambulance or another recognized provider, you qualify to complete a shortened Wilderness First Responder Recertification course. If your most recent WFR certificate has already expired, you will need to re-complete the full Wilderness First Responder course to obtain a new WFR certificate.
Q. I can't find my Wilderness First Responder Certificate. How can I get a replacement?
If you took your last Wilderness First Responder course with Medi-Pro Response Solutions or frontline First Aid, we likely have a record of your certificate on file. Just let us know that you need a replacement copy and we'll send it out to you by email. Make sure to tell us if your email address has changed since your last Wilderness First Responder course registration, or if you need the copy sent to a different email.
Q. Where do Wilderness First Responder guidelines come from?
The International Liason Committee on Resuscitation (ILCOR), and the corresponding Consensus on Science and Treatment Recommendations (CoSTR) task force groups constantly review and evaluate current Professional Medical Responder and Basic Life Support practices from data collected around the globe. ICLOR and CoSTR periodically produce documents which summarize their most recent findings, as well recommendations on what current emgergency paramedical practices should be continued, which should be changed, and what new practices should be adopted. Based on the findings in these documents, as well as other scientifically credible sources, individual Wilderness First Responder and Paramedic training providers such as the Canadian Red Cross produce their own evidence-based guidelines and educational delivery models.
In British Columbia, the paramedic profession is governed and regulated by BC Emergency Health Services (BCEHS) and the BC Emergency Medical Assistant's Licensing Board (EMALB). As such your Wilderness First Responder course will include many skills and protocols which are specific to British Columbia as dictated by BCEHS and EMALB which are updated frequently.
Q. Should I take an Wilderness First Responder course?
Canadian Red Cross Wilderness First Responder courses are appropriate for anyone who wants to learn the most up to date advanced first aid and CPR skills, to brush up on and expand on existing medical responder skills, or wants to improve their ability to respond with calm, assertive confidence in a medical emergency in a remote outdoor circumstance. You might need Wilderness First Responder certification to meet the requirements for an employment or educational opportunity, help out in your community, or just improve your first aid skills. Either way, a Wilderness First Responder course is a great place to start your training in an enjoyable and learner centered atmosphere. The training, skills, knowledge, certification, content and learning objectives included with a Canadian Red Cross Wilderness First Responder course is relevant for...
- Ecologists
- Adventure Racers
- Cyclists and Downhill Bikers
- Recreational Campers
- Remote Outdoor field workers
- Outdoor Guides
- Wilderness Trip Leaders
- Summer Camp leaders
- Geographic Surveyors
- Geologists
- Ski Guides
- Tour Guides
- School Trip leaders
- Search and Rescue personnel
- Ski Patrollers
- Mountain Bike Patrollers
- Water Quality Surveyors
- Hunting Guides
- Fishing Guides
- Forestry Workers
- Environmental Workers
- Travellers
- Campers and Backpackers
- Kayakers and River Guides
- Paddlers and Open Water Guides
- Mountaineers and Mountain Guides
- Park Rangers
You should always confirm specific course and certification requirements with your employer, educational institution or governing body before making your course selection. Medi-Pro First Aid can provide you with best practice recommendations based on industry standards, but cannot make a blanket guarantee that any particular First Aid/Medical Responder course will meet your individual requirements.
Q. What is Hands-Only CPR?
The baseline performance of bystander CPR includes continuous cycles of chest compressions combined with alternating ventilations/rescue breaths. The chest compressions pump blood from the heart and circulate it to vital organs. The rescue breaths put oxygen back into the lungs and bloodstream so that the blood being circulated is keeping cells alive. Ideally, an AED should be used as soon as possible as well.
Hands-Only CPR (also known a Compresssions-Only CPR) is an alternative which takes into account that a bystander may not feel safe or comfortable performing the rescue breathing component. Performing the chest compressions continuously, without providing rescue breaths, can still produce a positive outcome without the real or perceived risks associated with rescue breathing. Although not as statistically effective as traditional CPR, the application of Hands-Only CPR has been proven vastly superior to doing nothing, and can help ensure the patient is still viable when emergency crews arrive to perform more advanced procedures.
Wilderness First Responder Course Preparation
You will maximize your opportunities for success enjoyment through your Canadian Red Cross Wilderness First Responder course in Kelowna and Vancouver, BC if you review the basic expectations and arrive fully prepared, with your WFR Study Guide completed.
The more familiar you are with the online resources, educational supplements, printed text books, and WFR support materials at your disposal, the more likely you are to enjoy your WFR course and be successful in obtaining WFR certification and licensure.
Wilderness First Responder Study Guide
.jpg)
Access and complete our Wilderness First Responder Study Guide to help prepare you for your Wilderness First Responder course in Kelowna and Vancouver, BC. The WFR Study Guide has been developed to help prepare you for success and enjoyment in your BC Wilderness First Responder course.
There are two significant sources of information and WFR protocols for Wilderness First Responders training and practicing in British Columbia. The Canadian Red Cross provides you with a Nationally recognized WFR Program and Certification, following the content in the Emergency Care for Professional Responders reference manual. BC EMALB has jurisdiction over Provincial Licensing in BC, and has a few BC specific protocols, based on the EMALB Examination Guidelines and BCEHS Treatment Guidelines, that differ slightly from the national Canadian Red Cross program.
Completing the WFR Study Guide before starting your Wilderness First Responder course will help make sure you arrive familiar with the information and resources available to you. Your Wilderness First Responder course classroom sessions will center primarily on physical skills and hands-on practice and application, so the Study Guide will also help ensure that you have the background information and theory needed.
Wilderness First Responder Study Guide Sections:
- Section A: Text Book Corrections
- Section B: Certification and Licensing
- Section C: BC EMALB Jurisprudence
- Section D: EMALB Examination Guidelines
- Section 1: The Professional Responder
- Section 2: Responding to the Call
- Section 3: Infection Prevention and Control
- Section 4: Anatomy and Physiology
- Section 5: Assessment
- Section 6: Airway Management and Respiratory Emergencies
- Section 7: Circluatory Emergencies
- Section 8: Shock
- Section 9: Hemorrhage and Soft Tissue Trauma
- Section 10: Musculoskeletal Injuries
- Section 11: Chest, Abdominal and Pelvic Injuries
- Section 12: Head and Spinal Injuries
- Section 13: Acute and Chronic Illness
- Section 14: Poisoning
- Section 15: Environmental Illnesses
- Section 16: Pregnancy, Labour, and Delivery
- Section 17: Special Populations
- Section 18: Crisis Intervention
- Section 19: Reaching, Lifting, and Extricating Patients
- Section 20: Transportation
- Section 21: Multiple Casualty Incidents
- Section 22: Pharmacology
- Section 23: Marine Environment
- Section 24: Workplace
Emergency Care for Professional Responders
Canadian Red Cross Emergency Care for Professional Responders reference manual. Utilized by Wilderness First Responder course participants in Kelowna and Vancouver, BC.
The vast majority of the emergency medical skills, principles, guidelines and metrics you will learn and practice in your Canadian Red Cross Wilderness First Responder course are based on the Emergency Care for Professional Responders text book, which follows the Paramedic Association of Canada's (PAC) National Occupational Competency Profiles (NOCP).
The Canadian Red Cross Emergency Care for Professional Responders
reference manual is a 453 page, full-color text book with a soft red and white cover. Emergency Care for Professional Responders is available as a downloadable PDF, and in a printed edition. Electronic access to the PDF version is included with your Wilderness First Responder course registration, and you have the option to purchase a take-home printed copy as well.
The Canadian Red Cross Emergency Care for Professional Responders reference manual can also be purchased by anyone with an interest in the most current and scientifically valid evidence-based Emergency Medical Care practices in Canada.
Emergency Care Manual Contents:
- Professional Responder Training Levels
- Preceptorship
- Medical Oversight
- Communicating with the Medical Director
- Professional Responder Responsibilities
- Interpersonal Communication
- Self-Care
- Critical Incident Stress and Post-Traumatic Stress Disorder
- Legal and Ethical Issues
- Duty to Act
- Scope of Practice
- Abuse and Neglect
- Consent
- Refusal of Care
- Transfer of Care
- Documentation
- Communication
- Medical Terminology
- Preparing for the Emergency
- Response
- Equipment
- Plan of Action
- Communications
- Training
- Psychological Preparation
- Managing Hazards at the Emergency Scene
- Personal Safety
- Safety of Others
- Special Emergency Scenes
- Specific Scene Hazards
3. Infection Prevention and Control
- How Infections Occur
- Disease-Causing Pathogens
- How Diseases are Transmitted
- Epidemics and Pandemics
- Diseases that Cause Concern
- Immunization
- Preventing Disease Transmission
- Personal Hygeine
- Personal Protective Equipment (PPE)
- Engineering and Work Practice Controls
- Cleaning and Disinfecting Equipment
- Spill Management
- Exposure Control Plans
- If an Exposure Occurs
- Anatomical Terminology
- Body Cavities
- Body Systems
- The Cell
- Respiratory System
- Circulatory System
- Lymphatic System
- Immunological System
- Nervous System
- Musculoskeletal System
- Integumentary System
- Endocrine System
- Digestive System
- Genitourinary System
- Interrelationships of Body Systems
- How Injuries Occur
- Scene Assessment
- Primary Assessment
- Reassessment
- Secondary Assessment
- Treatment/Interventions
- Documentation of Findings
- Ongoing Assessment
6. Airway Management and Respiratory Emergencies
- Respiratory Pathophysiology
- Airway Obstruction
- Respiratory Conditions
- Assisted Ventilation
- Resuscitation Devices
- Resuscitation Masks
- Bag-Valve-Mask (BVM) Rescusitators
- Supplemental Oxygen
- Airway Adjuncts
- Oropharyngeal Airways
- Nasopharyngeal Airways
- Supraglottic Airways
- Suction
- Care for Respiratory Distress
- Care for Respiratory Arrest
- Cardiovascular Disease
- Angina
- Myocardial Infarction (MI)
- Congestive Heart Failure
- Cardiac Arrest
- Cardiopulmonary Resuscitation
- Compressions
- Team Approach
- Using a Defibrillator
- Special Resusciation Situations
- Post-Cardiac Arrest Care
- Cerbrovascular Accident (Stroke)
- Transient Ischemic Attack (TIA)
- CVA Assessment Scales
- Pathophysiology of Shock
- Types of Shock
- Stages of Shock
- Care for Shock
9. Hemorrhage and Soft Tissue Trauma
- Infection
- Dressings and Bandages
- Stitches and Sutures
- Tourniquets
- External Bleeding
- Internal Bleeding
- Open Wounds
- Closed Wounds
- Burns
- Major Soft Tissue Trauma
- Types of Musculoskeletal Injuries
- Splints
- Slings
- Signs and Symptoms of Musculoskeletal Injuries
- Upper Extremity Injuries
- Lower Extremity Injuries
11. Chest, Abdominal and Pelvic Injuries
- Chest Injuries
- Rib fractures
- Hemothorax
- Pneumothorax
- Subcutaneous Emphysema (SCE)
- Penetrating Chest Injuries
- Abdominal Injuries
- Evisceration
- Abdominal Aortic Aneurysm (AAA)
- Pelvic Injuries
- Pelvic Binding
- Genital Injuries
- Mechanism of Injury for Head and Spinal Injuries
- Head Injuries
- Skull fractures
- Objects Impaled in the Skull
- Injuries to the Brain
- Cerebral Hematoma
- Spinal Injuries
- Spinal Motion Restriction (SMR)
- Care for Serious Head and Spinal Injuries
- Rapid Extrication
- Removing Helmets and Other Equipment
13. Acute and Chronic Illnesses
- Altered Mental Status
- Syncope
- Diabetic Emergencies
- Seizures
- Types of Seizures
- Epilepsy
- Peritonitis
- Appendicitis
- Bowel Obstruction
- Gastroenteritis
- Kidney Stones
- Peptic Ulcers
- Gastrointestinal Bleeding (GI)
- Urinary Tract Infection (UTI)
- Poison Control Centres
- Recognizing Poisoning
- General Care for Poisoning Emergencies
- Ingested Poisons
- Inhaled Poisons
- Absorbed Poisons
- Injected Poisons
- Substance Misuse and Abuse
- Crowd Management Agents
- Temperature Homeostasis
- Heat-Related Illness
- Heat Cramps
- Heat Exhaustion
- Heat Stroke
- Cold-Related Illness
- Hypothermia
- frost Nip
- frostbite
- Drowning
- Cold-Water Immersion and Drowning
- High-Altitude Illness
- SCUBA-Related Illness
- Physiology
- Barotrauma of Descent
- Barotrauma of Ascent
16. Pregnancy, Labour, and Delivery
- Pregnancy
- The Birth Process
- Assessing Labour
- The Labour Process
- Preparing for Delivery
- Assisting with Delivery
- Caring for the Neonate and Mother
- Care and Assessment for the Neonate
- Caring for the Mother
- Midwives and Home Births
- Complications during Pregnancy
- Spontaneous Abortion
- Premature Labour
- Ectopic Pregnancy
- Third Trimester Bleeding
- Complications During Childbirth
- Prolapsed Cord
- Breech Birth
- Limb Presentation
- Multiple Births
- Pediatric Patients
- Stages of Development
- Anatomical and Physiological Differences
- Assessing the Pediatric Patient
- Other Pediatric Conditions
- Geriatric Patients
- Dementia and Alzheimer's Disease
- Osteoporosis
- Bariatric Patients
- Palliative Patients
- Patients with Disabilities
- Psychological Crisis
- Suicide
- Assault
- Death and Dying
- Mental Health Crises
- Anxiety
- Depression
- Psychosis
19. Reaching, Lifting, and Extricating Patients
- Gaining Entry to Buildings
- Motor Vehicles
- Stabilizing Vehicles
- Accessing the Patient
- Moving Patients
- Body Mechanics
- Stretchers and Lifting Devices
- Lifting and Moving a Stretcher
- Bariatric Patients
- Emergency Vehicle Maintenance and Safety Check
- Removing a Vehicle from Service
- Beginning and Ending a Shift
- Safe Vehicle Operation
- Air Medical Transportation
- Patient Considerations
- Landing Site Preparation
- Ground Safety Precautions
- Medical Evacuation from a Ship
- Preparing the Patient for Transfer
21. Multiple Casualty Incidents
- Organizing Resources
- Caring for the Ill or Injured
- Triage
- CBRNE Emergencies
- Types of Agents
- Methods of Dissemination
- Scene Assessment
- Establishing Perimeters
- Triage in a CBRNE Incident
- Control of Contaminated Casualties
- Transporting CBRNE Patients
- Psychological Impact of CBRNE Events
- Assisting with Medication vs Administering
- Six Rights of Medication
- Pharmacological Terminology
- Routes of Drug Administration
- Pharmacokinetics
- Pharmacodynamics
- Intravenous (IV) Therapy Maintenance
- Preparing a Drip Set and Solution
- Calculating IV Flow Rates
- Changing an IV Bag
- Complications
- Discontinuing an IV Bag
- How to Administer Medication Intranasally
- Guidelines for Injections
- Disinfection
- Maritime Occupational Health and Safety Regulations (MOHS)
- Sterilization Techniques
- Managing Dangers at the Scene
- Toxicological Hazards on Board a Ship
- Psychological Well-Being of Seafarers
- Medical Care of Rescued Persons
- Radio Medical Advice
- Transfer and Transport
- Marine Pharmacology
- Medications and Health Supplies Carried on Board
- Drugs Requiring Medical Advice
- Roles and Responsibilities of the Advanced First Aid Attendant
- Responsibilities of the Employer and Other Employees
- Return-to-Work Protocol
- Workplace First Aid Equipment
- Workplace First Aid Transportation
- Regulations and Documentation
- Workplace Occupational Health and Safety Regulations
- Workplace Hazardous Materials Information System
- Documentation
- Typical Workplace Injuries
- Workplace Injuries
- Appendix A: Abbreviations for Documentation
- Appendix B: Sample Ambulance Equipment List
- Appendix C: The Phonetic Alphabet
- Appendix D: Medical Terminology
Canadian Red Cross Wilderness First Aid Field Guide
.jpg)
The Canadian Red Cross Wilderness & Remote First Aid Field Guide is a smaller, more portable companion book to the Comprehensive Guide to First Aid. You will refer to the Wilderness & Remote First Aid Field Guide throughout your Canadian Red Cross Wilderness First Responder course in Kelowna, BC. A significant part of your Wilderness First Responder training involves familiarizing yourself with the Wilderness Field Guide, and learning how to use it as an on the spot reference when you encounter an emergency.
The information in the Canadian Red Cross Wilderness & Remote First Aid Field Guide follows the guidelines from the most currently recognized International Liaison Committee on Rescuscitation (ILCOR) and Canadian Consensus on Science and Treatment Recommendations (CoSTR) recommendations.
Your Canadian Red Cross certified Wilderness First Responder instructor will provide you with a classroom copy of the Wilderness & Remote First Aid Field Guide to utilize in your WFR course. You also have the option to purchase a take-home copy, to keep in your home First Aid kit, vehicle glove box, backpack, camper, boat or cabin. You might even decide to buy a few copies to keep in different locations. You can also download a PDF copy of the Wilderness & Remote First Aid Field Guide included with your course fees, and keep it stored for quick, easy access on your computer, laptop, tablet and smartphone. Wilderness & Remote First Aid Field Guide contents:
- Minor Emergency
- Major Emergency
- Critical Emergency
- Wilderness First Aid & Wilderness First Responder only
- Italicized Tips
- Getting Permission to Help
- Trip Plan
- Food and Personal Medications
- Six Rights of Medication
- Water
- Lowering the Risk of Infection
- Camp Set-Up
- Leave No Trace
- Sleep Or Rest
- Check
- Check the Scene
- Check the Person (Primary Assessment)
- Checking ABCs
- Recovery Position
- Secondary Assessment
- The SOAP Note
- Focused Examination
- Hands-On Check
- Shock
- Action Plan
- Death
- Backblows
- Abdominal Thrusts
- Chest Thrusts
- If you are by yourself and choking
- Baby
- Angina and Heart Attack
- Stroke
- Life-Threatening External Bleeding
- Tourniquets
- Life-Threatening Internal Bleeding
- Compression-Only CPR
- CPR Compression Depth
- Automated External Defibrillator (AED)
- Using an AED
- Respiratory Distress
- Asthma Attack
- Anaphylaxis
- Smoke Inhalation
- Bandaging Guidelines
- Infection Guidelines
- Bruises
- Cuts and Scrapes
- Scalp Injury
- Friction Blisters
- Impalement
- Removing an Object
- Splinters
- Fish Hooks
- Nosebleeds
- Knocked-Out Teeth
- Eye Injuries
- Ear Injuries
- Amputation
- Evisceration
- Chest Injuries
- Burns
- Burn Priority Level
Head, Neck and Spinal Injuries
- Removing a Helmet
- Concussion
- Moving a person with a Head, Neck, or Spinal Injury
- Improvised Heand and Spine Management Options
- Tarp Lift
- Spinal Motion Restriction
Bone, Muscle, and Joint Injuries
- Splints and Slings
- Pelvic Injuries
- Realigning Fractures
- Dislocation
- Digestive Illnesses
- Diabetic Emergency
- Seizures
- Mental Health Crisis
- Suicide
- Labour and Childbirth
Environmental Injuries or Illnesses
- Heat-Related Illnesses
- Cold-Related Illnesses
- Hypothermia
- Application of a Hypothermia Wrap
- Skin Frozen to Metal
- Water-Related Illnesses
- Cold Water Immersion
- What To Do: Rescue and Survival
- Self-Rescue: Open Water
- Self-Rescue: Breaking Through the Ice
- Rescuing Another Person
- Drowning
- Responsive Drowning Person
- Extremes in Atmospheric Pressure-Related Illnesses
- SCUBA-Related Illnesses
- Lightning Injuries
- Inhaled
- Swallowed
- Absorbed
- Injected
- Animal Bites
- Animal Stings
- Leeches
- Venomous Snakebites
- Venomous Spider Bites
- Tick Bites
- Basic Care
- Shelter, Fire, Food, and Water
- Body Positions and Movement
- Personal Hygeine
- Toileting Care
- Rest
- Extended Wound Care
- Abscess Draining
- Pain Management
- Psychological Care
- Documentation
- Waterproof Documentation
- Communicating the SOAP Note
Evacuation: Transporting the Ill or Injured Person
- Carries and Stretchers
- Carries
- Stretchers
- Getting Help
- Signalling
- Activate Professional Rescue
- Commercial Evacuation
Assessment and Decision Making Chart
Basic Life Support Field Guide
.jpg)
Canadian Red Cross Basic Life Support Field Guide. Utlized by BLS, WFR, WFR, Oxygen Therapy and Airway Management course students in Kelowna and Vancouver, BC.
The Canadian Red Cross Basic Life Support Field Guide reference manual is a pocket-sized, spiral bound 52 page, full-color text book with a soft red and white cover. The exterior cover and interior pages of the BLS Field Guide are made of a water resistant paper material, so you can keep it with you in the rain or wet environments without worry. The Basic Life Support Field Guide is available in PDF format as a downloadable resource for your mobile device, and in printed edition for Basic Life Support, Wilderness First Responder, Wilderness First Responder and Advanced First Aid course students.
The BLS Field Guide can also be purchased or downloaded by anyone with an interest in the most current and scientifically valid high-performance team based CPR-AED practices in Canada.
BLS Field Guide Contents:
Part 1. Introduction to Basic Life Support
- Basic Life Support Terminology
- Legal Issues
- Consent
- Implied Consent
- Responsive Patients
- Unresponsive Patients
- Children
- Abandonment
- Advance Directives
Part 2. Basic Life Support Skills
- Glove Removal
- Primary Assessment
- CPR
- Airway Obstruction
- Assisted Ventilation
- Anatomical Terminology
- Opening the Mouth
- Airway Adjuncts
- Suction
- Pulse Oximetry
- Pulse Oximeter Ranges and Values
- Supplemental Oxygen
- Oxygen Cylinders
- Oxygen Regulators
- Duration of Flow
- Oxygen Delivery Devices
- Administering Oxygen
- Special Considerations
- Trauma
- Hypothermia
- Opioid Overdose
- Anaphylaxis
- Six Rights of Medication
- High-Performance CPR
- Post-Cardiac Arrest Care
- High-Performance Team Communication
- Post-Event Debrief
.jpg)
Cheat Sheet for Canadian Red Cross Wilderness First Responder courses, in Kelowna and Vancouver, BC. Medi-Pro First Aid's Wilderness First Responder (WFR) Cheat Sheet will provide you with quick and easy access to some of the most critical and frequently referred to information throughout your Kelowna WFR Course.
The visually compelling Charts and Summaries can simplify the more complex principles and procedures you'll need to be familiar with as an Wilderness First Responder operating in British Columbia.
While most of the Wilderness First Responder Cheat Sheet is based on information extrapolated from the Canadian Red Cross Emergency Care for Professional Responders WFR text book, some of the information is based on the BC specific policies and guidelines stipulated by the British Columbia Emergency Medical Assistant's Licensing Board (BC EMALB) and BC Emergency Health Services (BCEHS). The Wilderness First Responder Cheat Sheet can be an invaluable resource for you to keep track of the specific local protocols that will help ensure sucess in your Wilderness First Responder course and throughout your corresponding examinations.
Wilderness First Responder Cheat Sheet contents include...
- WFR Patient Assessment Model
- CPR Compression to Ventilation Ratios
- High Performance "Pit Crew" CPR
- CPR in Transport (Treatable CPR)
- Oxygen Cylinder Calculations
- Oxygen Flow Rates
- Glasgow Coma Scale
- APGAR Assessment for Newborn Infants
- The 6-Rights of Medication
- Common Units of Measurement
- Assisted Ventilations
- BCEHS Treatment Guidelines Compared to National Occupational Competency Profiles
- Critical Findings
- Kendrick Extrication Device (KED) Strapping Sequence
- Glucogel Administration Guidelines
- Head-to-Toe Assessment Mnemonics
- Relevant SAMPLE and Mechanism of Injury Data
- Medical Terminology
- NEXUS Spinal Motion Restriction Decision Matrix
- Naloxone (Narcan) Administration Protocols
.jpg)
Downloads and online, web-based resources for Wilderness First Responder courses and BC EMALB requirements in Kelowna and Vancouver, BC. Wilderness First Responder certification training, and the provision of emergency medical care as a professional responder all involve far more that simply learning something once in the classroom. The wilderness medical responder profession is extremely dynamic and requires a lifetime committment to remaining up to date on the most current WFR protocols, guidelines, science, and practices.
This means that you will need to learn how to find the documented information and guidelines related to your Wilderness First Responder training and verify that what you remember learning is still considered a current practice. In addition to the documents and textbooks already outlined above, you will need to access and refer to several other online resources as you prepare to be successful throughout your Wilderness First Responder training.
Many of these resources can be downloaded and printed or saved, and some are only available online, through a desktop computer, laptop, or mobile web browser. Although you may find it convenient to download many of these documents and print them for easy reference, you should make a habit of frequently revisiting the source material online to make sure you are utilizing the most current materials.
Wilderness First Responder Certification Requirements
.jpg)
Our Wilderness First Responder courses are facilitated in a friendly, learner-centered environment, with the skills and principles presented in a simple and straight forward manner. Your Wilderness First Responder course Instructor will do everything possible to ensure that you meet national Canadian Red Cross, and provincial WorkSafe BC benchmarks for Wilderness First Responder certification and recognition.
Key first aid and CPR topics are presented in a distilled and relevant context, which makes them easy to understand and remember. A mix of interactive group activities and self-application make the first aid principles easy to understand and fun to learn.
Most of the course is dedicated to physical skills and hands-on learning which involve clear demonstrations immediately followed by opportunities to apply, practice, repeat and reinforce the first aid and CPR skills with realistic equipment.
In order to receive Canadian Red Cross Wilderness First Responder certification, which is valid for 3 years from date of completion and includes CPR level C, you must meet the following course attendance, performance and participation requirements.
- Attendance in 100% of the course
(this includes arriving, and returning from all breaks, on time) - Minimum 75% on a multiple choice written knowledge evaluation
(if needed, multiple attempts and reasonable accommodation are permitted) - Adherence to all classroom/facility health and safety guidelines
- Active participation in all activities, skills, and scenarios
- Respectful behaviour towards the Instructor all other participants
- Legible, accurate submission of your First & Last name and your preferred email address
(this is required for Medi-Pro to process your Certification through the Canadian Red Cross)
Personal Items to bring to your Wilderness First Responder Course
.jpg)
Bringing a few essential items with you to class can make the entire course more enjoyable. This added level of comfort can also help ensure you learn and retain the Wilderness First Responder and CPR skills, as well as meeting all the certification requirements as you participate.
Making sure you can see and hear your instructor, classmates and multi-media presentations is important. Although our Instructors will speak clearly and our video/projector screens are large enough to ensure full classroom visibility, you must bring any corrective eyewear or hearing aides (with fresh batteries) that you might need with you in your Wilderness First Responder course. In some cases you might need reading glasses for your Wilderness First Responder Field Guide and text/writing based activities, or you may need corrective lenses to clearly view the videos, slideshows and instructor-led first aid demonstrations.
If you normally require daily medications, you should definitely bring them with you to class, and adhere to your normal schedule. You might also find that your active participation in the first aid skills and activities throughout the day can increase your metabolic demands and the corresponding medication amounts. Medi-Pro recommends bringing double your normal amount of daily medications in case your needs increase or the session extends unavoidably.
Arriving fully prepared to remain warm, dry, nourished and comfortable for your Wilderness First Responder course will require careful planning and attention to detail. Once each course session begins, you will not have time to return for supplies that you forgot or misplaced.
If you become cold, wet, hungry or dehydrated throughout the session, your personal safety may become an overriding concern and your Instructor may have to discontinue your participation. The specific types of clothing and supplies required to maintain safe and comfortable participation will vary depending on personal preference, caloric demands, metabolism, the time of year, and daily weather patterns.
You can use Medi-Pro's suggested list of supplies and local weather predictions as a starting point for your preparations, but keep in mind that weather systems can change without warning and you know better than anyone what you will need to remain comfortable outside for extended periods.
The items listed here are intended to be referenced as minimum recommendations only, and should not be interpreted as a complete and exhaustive list of relevant and required equipment. It is better to bring supplies that you don't end up needing, than to need supplies that you didn't bring.
Hydration Supplies
- Small water bottle for drinking throughout the day
- Large water container to refill the small water bottle as required
- Bring double the amount of water/fluids you anticipate requiring for each session
- Electrolyte drinks/additives may be advisable
Food & Nutrition
- 6 substantial Snacks that can be consumed quickly, with little to no preparation required.
- 1 substantial Lunch
- 1 substantial "back-up" meal
- Cooler with ice to keep perishables fresh
- Any cooking supplies you require to prepare your food
- Small gas-burning camp stoves are permitted
- Camp/Cooking fires are forbidden unless explicitly permitted on a case-by-case basis
Clothing
- Hooded, water-resistant jacket
- Water-proof rain jacket/poncho
- 2 T-shirts
- 2 Long-sleeved shirts
- Thermal Fleece/Wool zip-up/pullover
- Hat with sun brim
- Toque/Thermal cap
- Water-resistant shell pants
- 2 pairs of Quick-dry pants
- Shorts (in warmer weather)
- Thermal underwear/longjohns
- Hiking boots/footwear with ankle and arch support
- Wool socks
- UV protective eyewear
Health & Safety Supplies
- Any prescription medications you require (double the normal daily amount)
- Prescription eyewear/contact lenses
- Flashlight/headlamp with spare batteries
- Mobile phone
- Sun screen
- Orthopedic equipment such as knee braces and ankle wraps
- Knee pads
- Hand soap/sanitizer
Personal Items
- Toilet Paper
- Chapstick
- Insect repellant
- Seat pad/portable chair
- Umbrella
- Knee pads
- Wet wipes
- Large towel
- Pen, paper and clipboard
- Bag/backpack large enough to carry all your supplies
Wilderness First Responder course Breaks and Lunch
.jpg)
Your first aid course will be conducted in an "Adult Learning" format, which means that you will be free to excuse yourself from the classroom at any time, if you need to use the washroom, answer a phone call/text, or attend to any other urgent matter that can't wait until the next scheduled break.
Medi-Pro administration and Instructors recognize that unanticipated circumstances may occur outside the classroom which require your immediate attention, but will ask that you limit these distractions to only those that are essential, and to minimize the disruption to other participants.
If you become thirsty or hungry, you are encouraged to keep yourself nourished and hydrated in the classroom, provided this does not interrupt hands-on activities or interfere with others' safety, participation and learning. There will also be formal breaks scheduled throughout the day, which can be utilized for communications, snacks, lunch and beverages.
- There will be a 15 minute break approximately every 2 hours, depending on classroom progress and participant pacing.
- You must arrive with enough water or other beverages to keep you hydrated throughout each classroom session.
- There will be one 30-minute Lunch break every day.
- Access to local stores and restaurants may be limited.
- You must arrive with enough ready-to-eat snacks and meals to keep you nourished throughout each classroom session.
- Medi-Pro recommends that you bring double the amount of food and drinks that you anticipate consuming throughout each session.
- Anticipate that warm weather will increase your hydration demands and cooler weather will increase your caloric demands.
- Use of electronics is discouraged except during breaks and when the Instructor deems it specifically appropriate.
- Smoking, including the use of vaporization products is limited to designated times and areas.
- Consumption of alcohol or illicit substances in the classroom, facility or grounds is prohibited.
- Impairment, as observed or presumed by the Instructor, will preclude you from participation and certification, regardless of the legality of any substances involved.
Wilderness First Responder course Hygeine and Attire
.jpg)
Participating in your Canadian Red Cross Wilderness First Responder course in Kelowna, BC will involve working in close proximity with your classmates, and in a wide variety of changing weather conditions. Respectful physical contact is an unavoidable component of hands-on First Aid training. Out of consideration for your classmates, please arrive with hygeine, and the comfort of others in mind.
Although it is impossible to define the term "appropriate" when it comes to clothing choices, there are few universal considerations. Slogans, logos, or images that could reasonably be categorized as objectively offensive or controversial must not be worn or displayed. Clothing which is soiled to the point that incidental contact may contaminate other clothing, equipment or furnishings are not acceptable in the classroom. Clothing or hygeine products which emit a strong odor may make it difficult for other participants to concentrate or enjoy the lessons and activities.
The health of all participants and staff is of paramount importance, so if you are feeling sick, or suspect that you may be contagious of any viral or bacterial infection, you must not attend the classroom. In cases of last minute cancellations related to unpredicted illness, Medi-Pro will make reasonable efforts to reschedule your course for a later date, when you are no longer sick/contagious.
Your clothing selections should accommodate the ability to adapt to temperature and environmental changes, including rain, wind, hot sunny weather, cold weather, snow, and wet ground. Please arrive with clothing, eyewear, and headwear that will allow you to continuously participate in relative comfort, and bring a backup set in case your first set becomes unwearable.
- Hygeine and beauty products should be unscented or lightly-scented only
- Jewellery or accessories that could cause injury or entaglement may need to be removed
(please do not bring expensive jewellery or irreplaceable heirlooms) - Longer hair needs to be secured in a way that prevents it from getting into others mouths and eyes
- Your clothing should allow you to participate with comfort and modesty
- Slogans or images that might be considered controversial, disrespectful or confrontational should be avoided
- Some types of clothing may restrict your ability to participate or compromise your classmates' comfort.
- Although it is impossible to define every aspect of the term "inappropriate" ahead of time, we ask that you take this into consideration when making your choices
- Wear layers that allow you quickly adapt to changing temperatures and activity levels
- Wear breathable fabrics with water repellancy on the outer layers
- Headear options should include something with a visor for sun protection, a warm toque in case of cold, and a water repellant hat with a large brim.
- Sunscreen and lipbalm may be necessary depending on your tolerance and weather conditions.
- Footwear should provide ankle stability and substantial treadgrip.
Physical Requirements for Wilderness First Responder
.jpg)
Participating in your Canadian Red Cross Wilderness First Responder course in Kelowna, BC will involve significant physical activity. If you have medical conditions, physical injuries or limitations that might compromise your ability to safely participate in these physical activities, you must notify your Instructor at the start of your course. Your Canadian Red Cross certified Instructor will make reasonable efforts to adapt and accomodate your limitations, but it is your responsibility to decide whether or not you can safely complete any particular task.
Your Canadian Red Cross Wilderness First Responder Instructor will balance the classroom between interactive theory components and hands-on physical activities, and you must actively participate in all the sections to successfully complete your Wilderness First Responder course. The physical requirements are not objectively intensive or difficult, but they do involve specific and repetitive movements. If you have any significant restrictions on your movement or exertion capacity, you should contact Medi-Pro well in advance of your scheduled course date to ensure that we can accommodate your limitations and provide the greatest opportunities for successful participation.
Physical activities typical of Canadian Red Cross Wilderness First Responder courses include...
- Working on the ground from kneeling and crouching positions
- Repeatedly laying on the ground during wet and cold weather
- Walking on rough, slippery and uneven terrain
- Walking up and down stairs, hills and slopes
- Rolling and lifting an adult sized classmate
- Performing CPR chest compressions on a CPR mannequin
- Using a pocket mask with a one-way valve to inflate the lungs of a CPR mannequin
- Tying simple knots
- Tearing medical tape
- Remaining outdoors for extended durations in all weather and conditions, including extreme heat, cold, rain and snow
- Kneeling on the ground
- Laying face-down on the ground
- Laying face-up on the ground
- Sitting for 15-30 minutes at at time
- Standing for 15-30 minutes at a time
Social Interaction in Wilderness First Responder Courses
WFR Course Skills & Principles
Get the most out of your Kelowna Wilderness First Responder course by familiarizing yourself with the WFR course content, schedule, skills and structure. The content, principles, skills and information covered in your Kelowna Wilderness First Responder training is broken into specific sections in your WFR printed materials and online resources. The extensive WFR level information provided in your Canadian Red Cross Emergency Care for Professional Responders reference manual is divided numerically into Sections 1 to 24, with Appendices alphabetically labelled. You are also provided with many other supplements, downloads and online resources which help put all this information into context, and provides guideance on how these skills and principles are specifically applied in British Columbia, as required by BCEHS and EMALB Licensing. These resources are referenced in your WFR Study Guide.
The classroom topics and content covered in each day of your Kelowna WFR course will generally correspond with specific sections of your Emergency Care Manual and supplemental resources. The sequence of topics covered in the WFR classroom will not necessarily follow the sequence in which they are presented throughout the Emergency Care for Professional Responders text. The daily schedule for every WFR course is subject to change and revision based on the needs of that particular WFR class.
- WFR concepts, principles, and skills are introduced in a simplified context and logical sequence.
- The WFR course starts with basic drills, and builds towards more complex scenarios with an emphasis on clinical decision making as participant skill levels and confidence improve.
- Stand-alone skill components are introduced and reinforced, then integrated into realistic situations and circumstances.
- Intensity, workload and student responsibilities increase as the WFR course progresses, with developing emphasis on clinical decision making abilities and adaptive skill application.
Introduction to First Aid Principles
.jpg)
Your Wilderness First Aid course will begin with an introduction to the basic principles of first aid, including how and when to call EMS/9-11, recognizing and overcoming barriers that might otherwise prevent or discourage you from providing help in an emergency, and the differences between providing first aid care as a well intentioned bystander compared the responsibilities of a designated workplace first aid attendant. The legal and ethical connotations of providing first aid as a bystander will become clear and you'll feel more comfortable with your role if the need arises.
You'll become familiar with universal Chain of Survival behaviours and the value of being prepared ahead of time in an emergency. An emphasis on injury prevention at home, work or play will hopefully allow you to adopt small, simple changes to your surroundings after the course which will help prevent the need for first aid care. In addition to learning and practicing how to use basic first aid equipment such as sterile dressings, pressure bandages, triangular bandages and automated external defibrillators, you'll also focus on the value and applications of mobile communication devices such as cellular phones as a powerful tool during a first aid event or any emergency. Introductory skills and principles covered in your Canadian Red Cross Wilderness First Aid course and materials include...
- About the Red Cross
- The Seven Fundamental Principles
- Humanity
- Impartiality
- Neutrality
- Independence
- Voluntary Service
- Unity
- Universality
- Preparing to Respond
- Barriers to Action
- Preparedness
- Chain of Survival Behaviours
- Being Prepared
- Injury Prevention
- Willingess to Help
- Emergency Medical Response System
- Calling 9-1-1
- Mobile Communications
- Role of the First Aider
- Employer First Aid Responsibilities
- Wilderness Emergency Response Plans
- Activating Emergency Response
- Bystander vs First Aid Attendant
- The Good Samaritan Act
Urban First Aid vs Wilderness First Aid
There are many differences between the urban First Aid principles that you would train for and utilize at home and in areas where 9-1-1/EMS services are readily available within a reasonable short timeframe. In urban circumstances, your role as a First Aider is generally limited to keeping the patient alive and as comfortable as possible while waiting in place for an ambulance to arrive and take over. In remote and wilderness settings, your First Aid responsibilities can increase dramatically by comparison, as well as the duration of time for which you are required to provide care for your patient. In remote circumstances, where emergency medical service is either unavailable or extremely delayed, you may need to consider First Aid and long term care interventions which would not be required or appropriate in an urban environment.
A sprained ankle in your front yard or on a downtown sidewalk will likely result in temporary discomfort and mild inconvenience in the big picture. However, suffering the same ankle sprain in an area that is inaccessible to any motor vehicles, and requires a 4-day hike to the nearest road access can have vastly different consequences. Not only does this injury prevent safe egress, but the rest of the group may become endangered as well, if supplies or weather patterns do not accommodate an extended trip duration. The immediate and ongoing decisions you'll have to make as a Wilderness First Aid responder may not only account for the injury itself, but the long term safety and survival of everyone involved. Some of the main skills and principles covered in your Canadian Red Cross Wilderness First Aid course and materials, regarding the differences between Urban and Wilderness First Aid include...
- Recognizing an Emergency
- Urban vs Wilderness First Aid Principles
- Geographically Remote Areas
- Technically Challenging Areas
- Accessing and Leaving Remote Areas
- Access to Definitive Medical Care
- Chain of Survival Behaviours
- Decision Making
- Personal and Group Concerns
- Use of Equipment
- Improvised and Commercial Equipment
- Environmental Factors
- How the Environment Affects Decisions
- Day Packs
- Trip Packs
Wilderness First Aid Planning
.jpg)
Wilderness First Aid training and principles extend far beyond simply reacting to injuries or illnesses as they occur. A trained and experienced Wilderness First Aid responder will start preparing and packing for potential injuries and medical emergencies while the trip is still in the planning stages. In many cases, the planning stage will involve obtaining information about the other individual members of trip, including any medical conditions, medications, allergies, emergency contacts, blood type, physical limitations, previous injuries, regular physician, and baseline vital signs such as resting heart rate and blood pressure. This information will help ensure the proper types and amounts of medications are brought, as well as a significant backup supply. A good rule of thumb is to pack double the amount of medication anticipated to be required.
It's also important to ensure that non-participating friends, family or administrators have a strong understanding of where the trip logistics including where it will begin, the waypoints and the end destination. If someone who is not travelling with the group will be making a pick-up, make sure everyone knows where and when this should take place. If a communication device is part of the trip equipment, you may want to arrange pre-designated messages and times to ensure outside resources are immediately deployed if an emergency causes delays or in case communications become disrupted. Don't forget to appoint another member of the group as the backup medical responder in case you end up in need of assistance yourself. Some of the main skills and principles covered in your Canadian Red Cross Wilderness First Aid course and materials, regarding planning and preparation include...
- Effective Leadership
- Legalities of First Aid
- Consent
- Preparing to be in a Wilderness or Remote Environment
- Trip Plan
- Trip Essentials
- Single-Day vs Multi-Day Trips
- Risk Assessment
- Assessing Human Factors
- Assessing Environmental Factors
- Food & Personal Medication
- Six Rights of Medication
- Seven Basic Body Needs
- Importance of Water
- Sleep
- Lowering the Risk of Infection
- How Infection Spreads
- Environmental Precautions
- PPE (Gloves)
- Camp Setup and Hygeine
- Preparing to Respond
- The Emergency Medical Services System
- After an Emergency
- Coping with Traumatic Events
.jpg)
The Patient Assessment Model is the foundation of your Wilderness First Responder training. The ability to intuitively follow a consistent and logical, yet flexible and adaptive process to assess your surroundings and the patient is the single most important key to being successful in your WFR course, your subsequent BC EMALB Licensing Evaluations, and most importantly in delivering high quality patient care as a professional medical responder.
A significant part of learning and practicing the WFR Patient Assessment Model also involves becoming familiar with the professional medical responder equipment available to you, and becoming increasingly proficient in their use. Some pieces of equipment, such as oxygen masks, blood pressure cuffs, stethoscopes and pulse oximeters are utilized during almost every patient interaction. Other types of equipment are bit more specialized, such as oropharyngeal airways (OPAs), nasopharyngeal airways (NPAs), and airway suction devices, and only utilized when necessary for patient assessment and care.
Although you will be provided with enough theory and background information to make use of these tools and processes, as much time as possible of your WFR course is dedicated to hands-on practice and reinforcement of these fundamental skills. Each time you practice applying these skills in a relevant and practical manner, the more proficient you will become and the more muscle memory you will develop for the future. Patient Assessment Model componenents, skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- WFR Assessment Model
- Scene Assessment
- WFR Equipment
- Paramedic Jump Kits
- WFR Scene Assessment
- WFR Primary Assessment
- WFR Secondary Assessment
- WFR Ongoing Assessment
- Patient Transport
- Medical Oversight
- Direct Medical Control
- Offline Medical Control
.jpg)
Assessing the scene that you are about to enter is the most important step in ensuring your own personal safety, as well as asserting and maintaining control over the situation to improve operational efficiency and provide quality patient care.
In some cases, such as an ongoing fire, hazardous materials spill, or confined space you may need to make a difficult but crucial decision to move or remain outside the hazardous area until more specialized rescue teams can mitigate the problem and/or bring the patient to you in a safe area. In other cases, such as a motor vehicle collision, you may be able to safely access the patient but require assistance from other agencies to extricate and transport the patient.
In all cases and at all times, you must maintain acute operational awareness of your surroundings and the changing conditions in which you are working. Taking a few extra seconds to meaningfully and thorougly evaluate the situation, and engaging all the required resources and personal protective equipment will save time overall and most importantly help ensure positive outcomes and the safety of everyone on the scene.
Scene Assessment, skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- How to perform a Scene Assessment
- How to assess the scene for hazards
- How to assess the environment of your surroundings
- How to assess the mechanism of injury
- How to assess the number of patients
- How to assess the need for additional resources on scene
- How diseases are transmitted
- Occupational Vaccinations and Booster Shots
- How to don and doff your Personal Protective Equipment (PPE)
- How to don and doff medical examination gloves
- How to don and doff protective eye-wear
- How to don and doff a face shield
- How to don and doff a medical examination gown
- How to call for Fire Rescue
- How to call for Haz-Mat Response
- How to call for Advanced Life Support
- How to call for Air Ambulance
- How to call for High Angle Technical Rescue
- How to call for Confined Space Rescue
- How to perform a seat-carry
- How to perform a clothing/blanket drag
- How to perform a walking assist
- The principle of Life-Over-Limb
.jpg)
The Primary Assessment survey is your first opportunity to check the patient for any obvious and immediately life-threatening injuries or conditions, and perform timely interventions to mitigate those injuries in a manner that stops or slows down any progressive decline in the patients condition. Airway, Breathing, and Circulation emergencies are generally the most crucial to identify and deal with in the first few minutes of your assessment. If there are any urgent problems with the upper airways, respiratory distress, or deadly external/internal bleeding, the Primary Assessment process gives you a systematic and efficient method to find and address those problems within a minute or two of arrival at the patient's side.
At the end of your Primary Assessment, you will pause to reflect on everything that you've already identified, review any outstanding or potentially life-threatening issues and initiate critical interventions such as OPA/NPA insertion, oxygen therapy, bleeding control, shock management and administration of medications as appropriate. You will also make your initial transport decision and determine whether immediate transport to definitive clinical care is a higher priority than continued and more thorough on-scene assessment. Although you will continuously receive, collect and consider new information as it changes or becomes available, the decisions you make in the first few minutes based on your Primary Assessment findings will set the tone for your overall patient care and transport priorities. Primary Patient Assessment, skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- How to conduct an WFR Primary Assessment
- How to measure and insert an Oropharyngeal Airway (OPA)
- How to measure and insert a Nasopharyngeal Airway (NPA)
- How to assemble an Oxygen cylinder and regulator
- How to use a Simple Oxygen Mask
- How to use a Non-Rebreather Oxygen Mask
- How to use a Nasal Canula
- How to place patients in the Recovery Position
- How to find and assess the Radial pulse
- How to find and assess the Carotid pulse
- How to check Skin condition
- How to perform an WFR Rapid Body Survey (RBS)
- Rapid Transport Category (RTC) criteria
- How to conduct the WFR Secondary Assessment with an Unresponsive Patient
- How to conduct the WFR Secondary Assessment with a Responsive Patient
.jpg)
The Secondary Assessment survey is conducted on scene when there are no urgent, life-threatening conditions which make rapid transport a higher priority. In cases of urgent transport, the Secondary Assessment is conducted enroute to the hospital, in the back of the ambulance. In some cases, where transport options are delayed or not available, you might conduct the Secondary Assessment on scene with life-threatening conditions, but transport to definitive clinical medical care is always more crucial when life-threatening injuries are present.
Components of a thorough, methodical and comprehensive Secondary Survey include an Interview of the patient and/or bystanders, family members, or witnesses, measurement of a complete set of Vital Signs, and a Head-to-Toe physical examination. Individually, each piece of data collected during the Secondary Assessment may not be significant or revelatory, however the information will collectively help form a clearer picture of all the potentially life-threatening, limb-threatening, or debilitating factors present and whether the patient's overall condition is improving or declining. Secondary Patient Assessment, skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- How to conduct an WFR Secondary Assessment
- How to measure and interpret SpO2 using a Pulse Oximeter
- How to perform a Capillary Refill circulation check
- How to conduct a patient interview following the S-A-M-P-L-E and O-P-Q-R-S-T mnemonic
- How to assess patient Signs and Symptoms
- How to assess patient Allergies
- How to assess patient Medications
- How to assess patient Previous relevant medical history
- How to assess patient's Last intake of food or fluids
- How to assess the Events leading up to current circumstances
- How to assess the Onset of pain or discomfort
- How to assess Provocation and Palliation of pain or discomfort
- How to assess the Qualities of pain or discomfort
- How to assess the Radiation of pain or discomfort from one anatomical area to another
- How to assess Severity of pain or discomfort on a subjective scale of 1-10
- How to assess the Timing of pain or discomfort
- How to assess Level of Responsiveness using the Glasgow Coma Scale (GCS)
- How to use a Stethoscope
- How to use a Sphagmomanometer (Blood Pressure Cuff)
- How to assess Blood Pressure using the Palpation method
- How to assess Blood Pressure using the Auscultation method
- How to assess Respiration rate, rhythm and character
- How to assess Radial Pulse rate, rhythm and character
- How and when to assess a patient's Vital Signs
- How to assess patient Pulse rate, rhythm, and character
- How to assess patient Respiratory rate, rhythm, and character
- How to assess patient Pupils for equal size and reaction to light
- How to assess patient Body Core Temperature
- How to Auscultate the chest to check for adventitious breathing sounds
- How to assess the Pedal pulse and Distal Extremity Circulation
- How to conduct an WFR Head-to-Toe Physical Examination
- How to conduct an WFR Head-to-Toe System Check
.jpg)
After you have conducted a thorough Secondary Assessment and treated any injuries or conditions identified, you will move into the Ongoing Assessment phase of your patient care. You will continuously reassess your surroundings and the patient's condition until the patient has been transferred to another (usually higher) level of care. This includes re-measuring the Vital Signs every 5 minutes if there are life-threatening conditions, or every 15 minutes if the injuries are minor in nature. You will also ask many of the S-A-M-P-L-E and O-P-Q-R-S-T Interview questions to see if the patient remembers anything new or is experiencing a change to their levels of discomfort. Continued, periodic reassessment will help you determine if there are any patterns in the changes to the patient's condition, such as gradually decreasing blood pressure or increasing oxygenation levels which can show overall improvement or decline and/or indicate specific underlying conditions.
The Ongoing Assessment phase also includes complete and accurate documentation of all your findings on a Patient Care Report. The report may be hand written on paper, or an electronic record stored and uploaded through a mobile device. Either way, an accurate and timely Patient Care Record forms a significant component of your overall patient care and contains information that may be potentially vital to the next level of care in forming an effective diagnosis and treatment plan. You will provide a brief but relevant verbal summary of your findings, actions and opinions regarding your patient when you hand them over to a higher level of medical treatment or another agency. Ongoing Assessment, skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- How to conduct an WFR Ongoing Assessment
- Patient Care Records and Reports
- Legal implications of Patient Care Records
- How to fill out a Patient Care Report
- How to ensure the Patient Care Report information is passed along
- Transferring patient care to another level of care or agency
- How to verbally transfer patient care using the S-B-A-R summary method
- How to summarize the overall patient care Situation
- How to summarize the overall patient care Background
- How to summarize your overall patient care Assessment and Actions taken
- How to summarize the overall patient care Results of those actions and interventions
.jpg)
Respiratory Illnesses such as asthma, COPD, pneumonia, emphysema, and congestive heart failure are very common medical emergencies that you may encounter as a paramedic/professional responder. Other medical conditions such as anaphylaxis and anxiety, and opioid overdose can also cause breathing problems and create respiratory distress. In your WFR course you will learn and practice a universal approach to providing patient care for someone experiencing Respiratory Distress, as well many techniques to mitigate specific respiratory problems as they are individually assessed.
The use of a pulse oximeter, supplemental oxygen therapy equipment, and particularly the efficient and effective use of a Bag-Valve-Mask (BVM) to assist ventilations and deliver high-flow oxygen are particularly relevant for a patient experiencing respiratory distress or respiratory arrest. In addition to these measures, you may commonly need to assist a patient with their medication such as ventolin, salbutamol, epinephrine, and/or benadryl. In the event that your patient is breathing too fast, too shallow, or too slowly to be effective, you will need to breath for them with a Bag-Valve-Mask, which is most efficient with two trained professional rescuers. Respiratory Distress and Respiratory Arrest skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- How to use a Bag-Valve-Mask (BVM) with one responder
- How to use a Bag-Valve-Mask with two responders
- How and when to Assist Ventilations
- How to provide care for a patient in respiratory arrest
- The 6 Rights of Medication
- How to recognize the signs and symptoms of Asthma
- How to provide care for a patient with Asthma
- How to assist patients with Asthma Inhalers
- How to recognize the signs and symptoms of Chronic Obstructive Pulmonary Disease (COPD)
- How to provide care for a patient in Respiratory Distress
- How to recognize the signs and symptoms of Anaphylactic Shock (Anaphylaxis)
- How to provide care for a patient experiencing Anaphylaxis
.jpg)
Cardiac arrest is another very common medical emergency, which requires the performance of Cardiopulmonary Resuscitation (CPR) and the use of an Automated External Defibrillator (AED) in an attempt to revive a patient without a pulse. Your WFR training course includes learning and practicing CPR at the Basic Life Support (BLS) level. BLS includes a team based "pit-crew" approach to CPR, the use of supplemental oxgyen, an AED, and high-performance roles performed and coordinated efficiently by each member of your medical response team.
High fidelity CPR begins with quick recognition of cardiac arrest followed by immediate chest compressions at a depth of at least 2 inches (for an adult) and at a rate of 100 - 120 compressions per minute. Compressions should be followed by the application and use of an Automated External Defibrillator (AED) which can administer an electrical shock to the heart and "reset" it to normal function when Ventricular Tachycardia or Ventricular Fibrillation are analyzed and detected. The next priority for quality CPR is providing ventilations/rescue breaths using a Bag-Valve-Mask with high-flow oxygen set to 15 liters per minute (lpm). The national standard for CPR compression to ventilation ratios is 30 compressions for every 2 breaths (30:2), however some specific agencies in BC may follow a regional guideline which stipulates a 10:1 ratio instead.
For purposes of performing CPR, anyone over the age of 9 (and/or the onset of puberty) is considered an Adult. Patients between the ages of 1 year and 9 years are considered Children, and patients under the age of 1 are considered Infants. There is an additional sub-set of Infants who are less than 28 days old referred to as Neonates. Although the basic principles of high fidelity CPR remain the same across patients of all ages, there are some logistical differences in performing CPR on smaller bodies. These differences include modified compressions, smaller ventilations, and performing CPR at a compression:ventilation ratio of 15:2. Basic Life Support and Cardiac Arrest management skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- How to perform CPR & AED for an Adult patient
- How to perform CPR & AED for a Child patient
- How to perform CPR & AED for an Infant patient
- How to perform CPR & AED for a Neonatal patient
- How to perform high-performance Pit Crew style CPR and AED
- How to perform Basic Life Support (BLS)
- How to provide care for a Responsive Choking Adult
- How to provide care for a Responsive Choking Child
- How to provide care for a Responsive Choking Infant
- How to use a manual airway suction device
- How to perform CPR & AED with an ongoing airway obstruction
.jpg)
The spinal cord is a cable of nerves extending from the base of the brain-stem down to the rest of the body, travelling through the vertebrae of the spinal column and branching out in nerve fibres to every area of the body. Signals that allow movement and function move through spinal cord from the brain to the rest of body, and sensory signals are carried from the nerve ends back to the brain through the same nerves. If an injury causes the spinal cord to become severed, the signals are no longer sent or received in either direction and sensory and motor deficits can permanently occur.
A significant portion of your WFR training course involves learning and practicing the prinicples of Spinal Motion Restriction (SMR), the Canadian C-Spine Rules, and the National Emergency X-Radiological Utilization Study (NEXUS) protocols which replaced the older Spinal Immobilization approach. The new SMR guidelines and accompanying modified NEXUS protocols adopted by BC EMALB provide paramedics with more options and flexibility to provide patient care when spinal cord injury is suspected, but the complex decision matrix requires memorization and practice.
You will also get lots of hands-on practice with spinal grips, skills, and equipment such as the trapezius grip, head grip, modified trap squeeze, jaw thrust, c-spine collars, robertson orthopedic stretchers (clamshells), spine boards, spider straps, head rolls, and rescue pads. The ability to mix and match a large "library" of skills and equipment as best suited to the specific circumstances will allow you provide the best patient care possible for suspected spinal injuries in any emergency. Spinal Motion Restriction tools, skills and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- Anatomy and Physiology of Spinal Cord Injuries
- Anatomy and Physiology of Head Injuries and Concussion
- How to recognize the signs and symptoms of Head and Spinal Injuries
- How to provide Spinal Motion Restriction (SMR) for patients with suspected Head or Spinal Injuries
- How to apply the Canadian C-Spine Rules in BC
- How to apply the modified Nexus C-Spine Rules in BC
- How to perform a Jaw Thrust
- How to perform a Trapezius Squeeze
- How to perform a Head Grip
- How to perform a Modified Trapezius Squeeze
- How to perform a Sternal-Spinal Grip in a supine position
- How to perform a Sternal-Spinal Grip in a lateral position
- How to align the Head into a Spinal-Neutral position
- How to measure and apply a C-Spine Hard Collar
- How to roll a patient from a supine to lateral position while maintaining Spinal Motion Restriction
- How to roll a patient from a prone position to a supine position while maintaining Spinal Motion Restriction
- How to secure a patient to a Spineboard with Spinal Motion Restriction precautions
- How to secure a patient to a Robertson Orthopedic Stretcher (Clamshell Stretcher) with Spinal Motion Restriction precautions
- How to provide patient assessment and care with Spinal Motion Restriction precautions
.jpg)
Deadly bleeding is another significant type of injury that you will encounter as a paramedic, and you will learn and practice the most current effective techniques to control external capillary, venous and arterial bleeding. The simplest approach to controlling deadly bleeding is direct pressure with a dressing and a bandage. Dressing is any clean (preferrably sterile and absorbent) material that is placed directly against the wound and blocks the bleeding, while a Bandage is any material used to surround the dressing, keep it clean and dry, and bind it securely in place with sufficient pressure to staunch the blood flow. Triangular bandages, speed straps and abdominal pads are some of the most commonly utilized tools to achieve direct pressure.
In some cases, where direct pressure is ineffective or impractical a tourniquet may be utilized to controll bleeding through Indirect Pressure. A tourniquet is placed upstream of the wound or amputation and bound tightly enough around the humerus or femur to squeeze the brachial or femoral artery shut against the bone. A tourniquet is usually only necessary in the most extreme injuries such as amputations. Deadly Bleeding tools, skills and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- Capillary Bleeding
- Venous Bleeding
- Arterial Bleeding
- Amputational Bleeding
- How to control deadly bleeding with direct pressure using a bandage and dressing
- Clinical bandages and dressings
- Improvised bandages and dressings
- The value of keeping a wound clean
- When to replace bandages and dressings
- How to recognize when direct pressure is ineffective
- How to control deadly bleeding with indirect pressure using a commercial tactical tourniquet
- How to control deadly bleeding with indirect pressure using an improvised tourniquet
- Where to place a tourniquet
- When to remove a tourniqet
.jpg)
fractures are injuries which cause any damage to bone structures, which can include cracking, chipping, splintering, complete breaks, and compound fractures where the broken bone ends protrude through the skin. Sprains are injuries to the ligaments which anchor the ends of two bones together, and usually involve stretching and/or tearing. Strains are injuries, which also usually involve stretching and/or tearing, to the tendons which hold muscles to bones. Dislocations are injuries that occur when two bone ends which normally connect are pulled out of alignment, usually involving a shoulder, knee, wrist, finger or toe.
When someone damages a bone or joint, the injury may be limited to just a fracture, sprain, strain or dislocation, but more often the injury is a combination of two or more of those conditions. For example, a fracture to an ankle bone will usually include some damage to the ligaments and tendons, and may even involve more than one bone. Regardless of the specific structures and tissues involved, an injury of this nature will usually present itself with universal signs and symptoms that include pain, tenderness, swelling and discoloration. It is not necessary to diagnose the specific types of inury/injuries to provide good first aid care.
Emergency medical care for fractures, sprains, strains and dislocations involves providing comfortable support for the injury, and preventing further aggravation or long-term complications. Injury stabilization and support is provided in the form of a splint, which can be created from many different materials and in many configuations. Ensuring that the patient remains as comfortable as possible, supporting the limb above and below the injury, and ensuring that circulation is not impaired are the main principles of splinting. It's important to note that although these types of injuries are not typically life-threatening, if the broken bones cut through the surrounding blood vessels, severe internal bleeding can occur. Fracture management and Splinting tools, skills and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- Musculoskeletal Anatomy & Physiology
- Signs and symptoms of Strains
- Signs and symptoms of Sprains
- Signs and symptoms of Closed fractures
- Signs and symptoms of Compound fractures
- Signs and symptoms of Dislocations
- Principles of splinting
- Assessing and maintaining distal circulation
- How and when to apply cold to a bone, muscle or joint injury
- How to apply a low arm sling with a triangular bandage
- How to apply a high arm sling with a triangular bandage
- How to apply a cross-arm transport sling with a triangular bandage
- How to splint lower arm injuries
- How to splint upper arm injuries
- How to splint shoulder injuries and dislocations
- How to use a flexible foam splint (SAM splint)
- How to use speed straps for splinting
- How to splint a wrist injury with a SAM splint
- How to splint leg injuries
- How to splint knee injuries
- How to create a pelvic girdle to splint hip injuries
- How to use a Kendrick Extrication Device (KED)
.jpg)
In many medical emergencies the single most effective and crucial interventions you can perform as a professional responder is to assist a patient with, or administer the appropriate medication. Some patients may have prescribed medication for specific medical conditions which have already been diagnosed by their physician. If you've followed some fundamental trip planning principles, that medication will be readily available with you in amounts exceeding the demand. In some cases a patient may require a medication for which they've never taken previously, and it may be up to you as the attending medical responder to determine how much medication to administer. Some medications are accompanied by clear indication/contraindication protocols which you can follow based on your observations and assessment of the patient. Other medications may require special permission from the patient themselves or from a supervising medical oversight service.
Following the "6 Rights" of Medication will help ensure you are providing the appropriate type and amount of medication following the proper administration technique. In all circumstances when either assisting with or administering medications to a patient it is extremely important to ensure that precise measurements and strict adherence to the parameters of the medication protocol are followed. Although medications can be a life saving intervention in the right circumstances, they can also cause severe side effects if misapplied. Pharmacology skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- Assisting with Medication vs Administering Medication
- Six Rights of Medication
- Pharmacological Terminology
- Drug Names
- Routes of Drug Administration
- Pharmacokinetics
- Drug Absorption
- Drug Distribution
- Biotransformation
- Excretion
- Pharmacodynamics
- Factors that Influence the Actions of Drugs
- Drug-Receptor Interaction
- Intravenous (IV) Therapy Maintenance
- Preparing a Drip Set and Solution
- Calculating IV Flow Rates
- Changing an IV Bag
- IV Complications
- Discontinuing an IV
- How to Administer Medication Intranasally
- Guidelines for Injections
- How to Prepare a Medication for Injection
- How to Administer a Subcutaneous Injection
- How to Give an Intradermal Injection
- How to Give an Intramuscular Injection
- Pain Management
- Disinfection
- Medical Oversight for Drug Administration
.jpg)
According to the Public Health Agency of Canada, Heart Disease is the second most common cause of death for Canadians. When the arteries that feed the heart muscle itself become occluded or blocked with cholesterol, plaque or blood clots the muscles of the heart become starved of oxygen and cannot function properly. This can lead to chronic Chest Pain known as Angina, where the heart muscle is continually starved, and eventually cause a Myocardial Infarction (Heart Attack) where the heart muscle actually dies from lack of blood and oxygen.
In your Canadian Red Cross Wilderness First Responder course, you'll learn how to recognize the most common signs and symptoms of a heart attack as well as the atypical/soft signs and symptoms mainly associated with heart attacks in women. In addition to taking the universal approach of treating for shock and keeping the person as calm, rested and comfortable as possible, you'll learn and practice how and when to assist with Acetylsalycilic Acid (ASA/Aspirin) tablets which are platelet inhibitors and an anti-inflammatory, and Nitroglycerin spray which is a blood vessel dilator.
BC Emergency Health Services and BC EMALB have very specific, Provincially applicable parameters for the administration of and provision of assistance with these medications. Heart Attack, Angina and Myocardial Infarction management skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- How to recognize the signs and symptoms of probable Angina
- How to recognize the signs and symptoms of a probable Heart Attack
- How to recognize the "Soft" signs and symptoms of a probable Heart Attack
- How to identify and recognize when to assist with Nitroglycerin spray for a patient with a prescription
- How assist with Acetylsalicylic Acid (ASA) for a patient experiencing signs and symptoms indicative of a probable Heart Attack
- How to provide assessment and care for a patient experiencing a probable Heart Attack
.jpg)
When a blood clot, embolism, plaque or aneurysm prevents adequate blood flow to the brain, a part of the brain tissue can starve or die, causing a stroke. In some cases the blood flow may resume before permanent damage occurs, which is commonly referred to as a Transient Ischemic Attack (TIA). The longer the blood flow is disrupted the more brain tissue dies and the more dramatic and permanent the damage becomes. As the left side of the brain controls the right side of the body, and the right side of the brain controls the left side of the body, the physical effects/deficits created by the stroke are usually seen on the opposite side of the affected brain.
Early recognition of the signs and symptoms of a potential Stroke, including sudden headache, one-sided weakness/paralysis, dizziness, confusion and slurred speech, and swift transport to definitive clinical medical care are the most important steps to prevent or mitigate permanent brain damage once a stroke has occured. When stroke-like signs and symptoms abate and resolve themselves shortly after ocurring, this is usually referred to as a Transient Ischemic Attack (TIA), however it is unlikely that you will be able to definitively diagnose between a Stroke and TIA on scene. The sooner a suspected Stroke patient gets to the hospital and receives advanced medical treatment and medications, the less brain function they will lose and the greater their chances of survival and fuller recovery. Stroke and Transient Ischemic Attack management skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- How to identify and recognize the signs and symptoms of a probable Transient Ischemic Attack (TIA)
- How to identify and recognize the signs and symptoms of a probable Stroke
- Field tools for assessing Stroke
- How to utilize and apply the Cincinnati Stroke Scale
- How to utilize and apply the F-A-S-T Stroke assessment tool
- The importance of urgent transport for Stroke patients
- Positioning Stroke patients for transport
- How to provide assessment and care for a patient experiencing a probable Stroke or TIA
.jpg)
Every cell in the body requires a continuous supply of sugar (glucose) to function normally, with a greater demand for glucose accompanying greater exertion. The harder the body, and it's cells work, the more glucose they require. When our body digests food, many of the nutrients are broken down into glucose, which is subsequently absorbed into the blood stream for distribution to the cells. When cells require glucose, the pancreas releases an appropriate amount of insulin to facilitate transporting the approriate amount of glucose from the blood stream into the cells for energy.
Diabetes is a condition in which the pancreas is unable to produce either any insulin or enough insulin, or the cells are resistant to insulin as a glucose transporter. In Type I Diabetes, this condition is present from birth or early childhood, while Type II Diabetes develops later in life as an adult. Regardless of whether Type I or Type II Diabetes is present, the essential problem created is an imbalance of glucose and insulin available in the bloodstream compared to cellular demand for energy.
Many people with Diabetes of both types take synthetic insulin by injection, in an attempt to match glucose transport with cellular demand, but this is a very delicate balance requiring precise amounts compared to precise exertion levels. It is very common for someone with Diabetes to end up with blood glucose levels that are too low to support cellular function (Hypoglycemia) or blood glucose levels that are too high (Hyperglycemia) for the body to process efficiently. Of the two potential states, Hypoglycemia generally develops much more rapidly and is more immediately life-threatening. Diabetic Emergency management skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- The relationship between Insulin and Glucose
- The relationship between cellular function and blood glucose levels
- Type I Diabetes
- Type II Diabetes
- How to recognize the signs and symptoms of a Diabetic Emergency
- How to identify and recognize Hypoglycemia
- How to identify and recognize Hyperglycemia
- How to administer oral glucose to a patient experiencing confirmed Hypoglycemia
- How to provide care for an unresponsive patient with suspected Hypoglycemia
- How to provide assessment and care for a patient experiencing a Diabetic Emergency
.jpg)
Seizures can occur when the electrical signals travelling through and across the brain start to misfire or get re-routed to unintended destinations. There are many types of medical conditions and injuries that can lead to seizures including Stroke, TIA, Head Injury, Concussion, Epilepsy, Brain Tumors, Diabetes (Hypoglycemia), and Hyperthermia. Basically, anything that disrupts the normal function of the brain can potentially cause a seizure. With pediatric or infant patients in particular, it is very common for a high fever to induce febrile seizures.
Seizures usually take place through several different stages, which may or may not appear distinct and sequential. The "Aura" phase of a seizure most often manifests as strange sensation similar to deja vu, out-of-body or other sensations inconsistent with surroundings. Someone who has experienced a seizure before may recognize the sensations that accompany the aural phase and alert others to the impending event. The Tonic-Clonic phase of a seizure most often involves uncontrolled muscle convulsions and decreased responsiveness which usually last up to a few minutes. During the Tonic-Clonic phase, the seizing patient may also present with irregular breathing due to interference with the muscles involved in respiration, and vomit, foam or saliva accumulating in the mouth which can obstruct the airway. Seizures that last more than a few minutes, or seizures that occur back-to-back with no recovery time in between are referred to as Status Epilepticus and indicate an urgent medical emergency.
When the Tonic-Clonic muscle convulsions cease, the patient usually enters the Post-Ictal phase of the seizure during which they gradually regain consciousness, experience extreme fatigue and may or may not recall the previous moments leading up to and during the event. Some seizures, known as Focal Seizures do not involve muscle convulsions, but instead cause a period of trance-like decreased levels of responsiveness and can be more difficult to assess.
Regardless of the specific cause, your main patient care priorities during the tonic-clonic phase of a seizure involve taking whatever measures are necessary to create and maintain a safe space around the patient to reduce the risk of physical injury caused by the convulsions. In some cases you may need to move the patient away from a set of stairs or body of water to prevent a fall or drowning, but for the most part you will avoid physically contacting or restraining the patient until the seizure has concluded. Seizure management skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- Signs & Symptoms of Seizures
- Causes of Seizures
- Epileptic Seizures
- Status Epilepticus
- Phases of a Seizure
- Aural Phase of a Seizure
- Tonic-Clonic Phase of a Seizure
- Post-Ictal Phase of a Seizure
- Focal Seizures
- First Aid for Seizures
- Febrile Seizures
- Pediatric patients with high fever
- Patient care during a seizure
- Airway and respiratory concerns during a seizure
.png)
Burns are among the most painful type of injury, and are generally classified into 3 categories based on the depth of tissues affected. Superficial/First Degree burns only affect the outer epidermal layer of the skin, and are usually accompanied by painful reddened areas. Partial Thickness/Second Degree burns involve the deeper tissues of the dermis as well as the outer epidermal layers, and are generally identified by pain, blisters, redness and thick peels of skin. Full Thickness/Third Degree burns usually cause blackened, charred skin and tissue which may extend all the way down to the fatty layers, muscles and even bone.
Burns can become immediately life-threatening if they affect the airways and/or impair breathing, which is particularly common with inhalation injuries from being inside a burning building or breathing in chemical fumes. The most commonly life-threatening aspect of burn injuries is the rapid onset of infection and subsequent septic shock. This occurs because the skin which normally protects internal tissues and structures from infection is removed or damaged allowing bacteria to rapidly and overwhelmingly permeate the body's systems.
Some of the most important aspects of providing emergency medical care for burn injuries that you will learn and practice in your WFR course include ensuring your own safety (in particular when dealing with chemical or electrical burns), cooling the burn to prevent further tissue damage, and protecting the burned areas from infection with dry and sterile/clean dressings. Wet fabric will wick dirt and bacteria through to the tissues, so a burn is not protected unless the coverings are clean and dry.
One of the most effective methods to cool a burn, and therefore prevent the residual heat from creating more extensive burns to the surrounding tissues, is to apply cool, gently flowing sterile water or saline solution over the burned areas. Care must be taken not to further traumatize the damaged tissues, and ensure that the body core temperature is not lowered to a hypothermic state. Once the tissues have been cooled and the residual heat removed, the burn can be covered to prevent infection. BCEHS and BC EMALB stipulate Provincial emergency care regulations which limit the time spent cooling a burn on scene to 3 minutes, with any further cooling conducted in transport as appropriate. Burn Care skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- How to identify and recognize Superficial (First Degree) burns
- How to identify and recognize Partial Thickness (Second Degree) burns
- How to identify and recognize Full Thickness (Third Degree) burns
- The Rule of Nines for Adult patients
- The Rule of Nines for Pediatric patients
- Estimating Burn Percentage
- Burns requiring urgent transport
- Cooling a burn
- Covering burns to prevent infection
- Burn Dressings
- Burn Blankets
- Inhalation Injuries
- Pain management for burns
- How to provide assessment and care for a patient with burns
.jpg)
Trauma Management includes assessment and care for a wide range of physical injuries which can range from inconvenient and painful to immediately life-threatening. Very often the most urgent and critical aspect of a truamatic injury is not the most visible component, but the underlying interference with normal body system functions, or internal complications that can accompany the obvious physical damage. For example, the puncuture hole of a sucking chest wound may only be a few centimeters in diameter, with relatively minimal external hemhorrage but the increasing amount blood and air becoming trapped inside the pleural cavity of the chest wall create a tension pneumothorax which will eventually prevent the lungs from expanding and restrict heart contractions.
Some of the most common types of traumatic injury that you will learn about and practice treating in your WFR course include Sucking Chest Wounds, Peumothorax, Hemothorax, Crush Injury, Harness Syndrome, Compartment Syndrome, Pelvic fracture, Flail Chest, Evisceration, Impaled Objects and Amputations. In almost all instances of these kinds of trauma, the underlying complications are usually more serious than the obvious external physical damage. Most of the immediate care that you provide for patients with truamatic injuries will focus on preventing further harm and mitigating the accompanying life-threatening complications.
You will learn and practice the application of a vented occlusive dressing over a sucking chest wound to mitigate the onset of tension pneumothorax, the application of a pelvic binder/girdle to prevent broken pelvic bones from lacerating abdominal organs during transport. Crush Injury and/or Harness Syndrome require a coordinated and rapid combination of extrication and immediate transport with supplemental intravenous fluids to counteract septic shock, while eviscerations require the application of multiple coverings over the exposed organs with a mix of absorbent, non-stick, moistened, non-permeable and insulatory layers. Traumatic Injury management skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- How to identify and recognize the signs and symptoms of an Amputation
- How to provide assessment and care for a patient with an Amputation
- Complete amputations
- Partial amputations
- How to identify and recognize the signs and symptoms of an Impaled Object
- Stabilizing an impaled object in place
- How to provide assessment and care for a patient with an Impaled Object
- How to identify and recognize the signs and symptoms of a suspected Pelvic fracture
- How to create a pelvic girdle
- How to utilize a commercial pelvic binder
- How to provide assessment and care for a patient with a suspected Pelvic fracture
- How to identify and recognize the signs and symptoms of an Evisceration
- How to provide assessment and care for a patient with an Evisceration
- How to identify and recognize the signs and symptoms of a Sucking Chest Wound
- Open Pneumothorax
- Closed Pneumothorax
- Spontaneous Pneumothorax
- Traumatic Pneumothorax
- How to provide assessment and care for a patient with a Tension Pnuemothorax
- How to identify and recognize the signs and symptoms of a Tension Pnuemothorax
- Tracheal Shift
- Jugular Vein Distension
- How to provide assessment and care for a patient with fractured ribs
- How to identify and recognize the signs and symptoms of fractured ribs
- How to provide assessment and care for a patient with a Flail Chest
- How to identify and recognize the signs and symptoms of a Flail Chest
- How to identify and recognize the signs and symptoms of Crush Injury
- How to identify and recognize the signs and symptoms of Harness Syndrome
.jpeg)
The ongoing Opioid Overdose Crisis is one of the most lethal, large scale and persistent Canadian public health crises in the past few decades. With the recent deregulation of the Opioid Antagonist drug Naloxone (Narcan), many agencies have made emergency Narcan Overdose/Poisoning kits available to the public and especially the most vulnerable populations. Fentanyl / Carfentanil misuse comprises the vast majority of Opioid overdose and fatalities, but there are many other opiates and harmful drugs as well.
Administering Narcan, in either intramuscular or intrnasal form can temporarily alleviate the most life-threatening aspects of Opioid overdose, such as respiratory arrest and unresponsiveness, but it does not completely remove the poison from the person's system. The opioids will remain in the system after the Naloxone has dissipated, so it is vital that someone receives definitive clinical medical care as soon as possible following the overdose and subsequent Narcan administration.
The signs and symptoms of a patient who is experiencing Opioid Overdose/Poisoning will generally involve the "Toxidrome" of opioid overdose including decreased level of responsiveness, absent or inadequate respirations, and pinpoint pupils. The depressed respirations that typically accompany opioid overdose will also reduce the patient's blood oxygen levels (SpO2) to dangerously low levels. In most cases, you will place a higher priority on securing airway patency, supplementing their oxygen levels and assisting ventilations, or even performing CPR, than the immediate administration of Naloxone.
The administration of Naloxone, once appropriate, may further support these critical interventions by increasing the patient's level of conciousness and/or improving their natural respiration rate, rhythm and character. Although multiple doses of Naloxone, at increasing dosages, may be required for optimal patient care, it is not necessary to completely reverse all the effects of the opoiod or achieve full patient responsiveness, as long as the airway remains clear and adequate respirations resume.
As an Wilderness First Responder you are also likely to encounter many other forms of poisoning and overdose such as household products, workplace chemicals, alcholol, barbituates, depressants, and stimulants which are not specifically related to opiates and therefore rendering Naloxone ineffective and contraindicated. Opioid Overdose and Poisoning skills, tools and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- Types of Poisons
- Types of Drugs
- Types of Chemicals
- Household Products
- Workplace Chemicals
- Workplace Hazardous Materials Information System (WHMIS)
- Safety Data Sheets
- Poison Control Centers
- Ingested Poisons
- Inhaled Poisons
- Injected Poisons
- Absorbed Poisons
- Substance Misuse
- Substance Abuse
- Overdose and Poisoning
- Fentanyl and Carfentanil
- Opioid Overdose Crisis
- Deregulation of Naloxone
- Public Access NARCAN (Naloxone) Kits
- The Toxidrome of Opioid Overdose
- How to identify and recognize the general signs and symptoms of a suspected Overdose
- How to provide assessment and care for a patient experiencing signs and symptoms indicative of a suspected Overdose
- How to identify and recognize the signs and symptoms of an Opioid Overdose
- Intramuscular Narcan Administration
- Intranasal Naloxone Administration
- Narcan / Naloxone doseages
- How to identify and recognize the Indications to administer Naloxone (Narcan) to a patient experiencing a suspected Opioid Overdose
.jpg)
Childbirth is a natural event which most often takes place as planned and predicted, without complications. However, when childbirth occurs ahead of schedule, unexpectedly, or under exigent circumstances, it can become one of the most stressful yet rewarding types of medical emergency you respond to as a paramedic or firefighter. Your WFR course and materials provides you with a basic understanding of childbirth, and how to provide medical assistance to the mother during labour and the birthing process.
You'll learn about pregnancy, and the stages of labour and childbirth, as well as universal steps to assist with delivery and make the mother, family members and newborn as comfortable and safe as possible throughout the birthing process. In the event of complications, you'll be familiar the most common underlying conditions which precipitate emergencies during the childbirthing process and which interventions are appropriate for each circumstance. Some of the most common pregnancy complications include spontaneous abortion, premature labour, ectopic pregnancy, and third trimester bleeding, and common childbirth complications include prolapsed cord, breech birth, limb presentation, and multiple births.
Once the newborn has been delivered, you will utilize the APGAR neonatal assessment system and provide any addtional care or intervention as required. In the event that a newborn (neonate) has a brachial pulse rate of less than 60 bpm, you will start CPR without an AED. The placenta will arrive within a few minutes of the infant, and should be kept warm and handled gently. The mother will also require care including interventions any ongoing or excessive hemorrhage. Emergency Childbirth tools, skills and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- Complications of Pregnancy
- Signs & Symptoms of Spontaneous Abortion
- Signs & Symptoms of Premature Labour
- Signs & Symptoms of Ectopic Pregnancy
- Signs & Symptoms of Third Trimester Bleeding
- The stages of Labour
- How to assess the stages of Labour
- Signs & Symptoms of Braxton Hicks Contractions
- Labour Stage One (Preparation)
- Labour Stage Two (Newborn Delivery)
- Labour Stage Three (Placenta Delivery)
- Labour Stage Four (Stabilization)
- The stages of the Birth Process
- How to assist with delivery of a baby
- Medical Complications of Emergency Childbirth
- Signs, Symptoms and Complications of Prolapsed Cord
- Signs, Symptoms and Complications of Breech Birth
- Signs, Symptoms and Complications of Limb Presentation
- Signs, Symptoms and Complications of Multiple Births
- Signs, Symptoms and Complications of Postpartum Bleeding
- How to provide medical care for a Neonate
- How to assess a Neonate using the APGAR systam
- Assessing Neonatal Alertness
- Assessing Neonatal Pulse
- Assessing Neonatal Grimace
- Assessing Neonatal Appearance
- Assessing Neonatal Respiration
- How to provide medical care for the Mother of a newborn
- Midwives and Doulas
- Planned and Unplanned Home Births
.jpg)
Although the phrases Multiple/Mass Casualty Incident (MCI) and Triage are often used interchangeably, they are distinct and separate terms. A multiple casualty incident describes any situation where two or more patients are injured, sick or otherwise require medical attention at the same time in the same vicinity. Vehicle accidents (particularly those involving passenger vehicles), hurricanes, tornados, earthquakes, building collapse, and chemical, biological radiological, nuclear, explosive (CBRNE) incidents are examples of circumstances that commonly create multiple casualty incidents. When patients/casualties outnumber available medical responders, Triage becomes necessary to avoid spending more time with any one patient than is absolutely necessary.
Triage is any rapid and efficient process of assessing multiple patients and quickly determining which require immediate care, which can wait, and which are already beyond saving. Most triage systems utilize a standardized color coding to identify four standardized patient categories. The color "Black" is utilized to identify patients who are already deceased or whose injuries are incompatible with life and will obviously outperform the available resources. The color "Red" is utilized to identify patients with immediately life-threatening injuries or conditions and for whom the application of critical interventions will create a more favourable outcome. The color "Yellow" is utilized to identify patients with injuries that are not immediately life-threatening but render the person unable/unsafe to move or walk without assistance. The color "Green" is utilized to identify patients who are uninjured, or whose injuries are not life-threatening and do not impede self-ambulation.
Color coding can be applied using a wide range of tools including markers, pre-coded tags, color coded flagging tape, color coded tarps, or spray paint to name a few. The assessment process utilized to rapidly determine which patient's are in which category is usually a variation of the primary assessment model, with strong emphasis on speed and efficency. In some cases, just calling out to a crowd and asking everyone who is capable to walk to a "Green" area may save time assessing patients without life-threatening injuries. In order to be effective, Triage depends on making instant decisions and spending only enough time with any given patient to ensure that they can sustain life a while longer. The more time that is spent on one patient, the longer another waits without assessment or treatment of any kind. It's important to keep in mind that Triage decisions are always extremely subjective and extended debate about any one decision defeats the purpose. It is also vital to maintain situational awareness and remain alert to new or unseen hazards related to the underlying causes of the multiple casualty incident. Multiple Casualty Incident and Triage tools, skills and principles covered in your Canadian Red Cross Wilderness First Responder course and materials include...
- Factors in Multiple Casualty Incidents
- When patients outnumber rescuers
- When to initiate Triage
- Assigning a Triage Officer
- The START system of Triage
- Simple Triage and Rapid Treatment (START)
- Triage Assessment Model
- Colour Coding Tools
- How to identify triage patients who are deceased or beyond saving
- How to identify triage patients with immediately life-threatening injuries or conditions
- How to identify triage patients with non-life-threatening injuries
- How to identify triage patients who are unable to move themselves safely
- Chemical, Biological, Radiological, Nuclear, Explosive (CBRNE) events
- Emergency Wash-Down Procedures
- Incident Command System (ICS)
- Incident Management System (IMS)
- Multi-Agency Responses
.jpg)
Nobody would dispute that professional football and hockey players are exposed to exponentially more physical trauma on a daily basis than the average person. Correspondingly, these elite athletes also incur physical injuries at greater freqency and of greater severity than most. Therefore, professional athletes adopt disciplined regimens of preventative physical training and immediately seek physical therapy to restore normal function when injuries occur, in order to secure a long and healthy career. A professional athlete is not disqualified from competing simply because their bones are not unbreakable, nor are they stigmatized for sensibly seeking expert medical treatment to heal.
Professional medical responders must acknowledge that they are similarly exposed to exaggerated levels of emotional and psychological trauma, and take the same attitude and approach as professional athletes do towards prevention, treatment and self-care. Having frequent, normalized conversations about the normal reactions to abnormal situations and circumstances that Wilderness First Responders are exposed to on a regular basis, which challenge deeply held values, should be no different than discussing a broken ankle or sprained knee. Emergency responders should not expect themselves or others to be immune to the effects of mental stress any more than a football player is expected to have unbreakable bones.
Long term psychological health can be facilitated by adopting an overall healthy lifestyle that includes regular and sufficient sleep, proper nutrition and regular exercise accompanied by as much time as possible doing enjoyable activities with friends and family. It will also likely be necessary to acknowledge the presence of Occupational Stress Injury (OSI) and seek whatever professional resources are necessary to prevent long-term disability. You cannot take proper care of your patients (at least not for long) if you do not take responsiblity for and proper care of your own physical and mental health. A lifestyle that promotes long-term mental and physical wellness includes...
- Healthy eating habits that include a sensible balance of nutritional and dietary needs
- A structured and disciplined approach to sufficient sleep cycles
- Regular exercise and activities which build strength and endurance
- Normalized ongoing conversations about exposure to abnormal circumstances
- Ample and time with friends and family spent on enjoyable activities
- Maintaining current training and education to ensure you are performing your duties responsibly
- Ongoing education about Occupational Stress Injury (OSI)
- Professional counseling or medical assistance when needed
- Acceptance that you are not immune to stress
- Acceptance that recovery may not occur as quickly as you like
- Acceptance that everyone reacts differently to the same circumstances and that all reactions are "normal".
- Self-awareness of the signs and symptoms of cumulative or acute Occupational Stress Injury (OSI)
- Continuous and ongoing access to local, Provincial, Federal or employer specific Occupational Stress Injury resources
Wilderness First Aid for Wildlife and Environmental Illnesses & Injuries
.jpeg)
The Canadian outdoors have a lot to offer, whether you are simply enjoying a walk in the local park, gardening in your back yard, or trekking up mountain passes to spectacular lakes and glaciers. However, the outdoor environment also poses some hazards if you are unaware or unprepared. Extreme cold and/or heat are two of the most pervasive and persistent factors that can create injury or health hazards, but there a several simple steps you can take to prevent your body core temperature from raising too low or too high. Proper clothing layers, pre-emptive hydration and nutrition, as well as vigilance for early signs of hypothermia or hyperthermia will mitigate most of the dangers and prevent the need for first aid measures.
Some local plant life can create injury and illness as well, ranging from minor itching to severe blistering and infection, and poisoning if ingested. The most reliable way to prevent unwanted exposure to plant toxins is to recognize the dangerous types and avoid them. Long sleeves and full-length pants can help prevent direct skin contact with nettles and barbs, and regular use of sun screen can reduce the effects of UV activated toxins such as those contained in Devil's Club/Hogsweed.
Although relatively rare, some types of local wildlife such as insects, spiders, snakes, scavengers, and large predators can pose a risk of significant injury or even death. The effects of the sting of some insects such as wasps or scorpions can range from mild irritation to anaphylaxis, while poisons from the bite of a brown recluse spider, black widow, or a rattlesnake can become fatal if the envenomation is high enough. Small animals such as racoons may appear cute and harmless, but may also carry infectious disease such as rabies, and large predator animals can create significant physical trauma when provoked or hungry. Environmental injury skills and principles covered in your Canadian Red Cross Wilderness First Aid course and materials include...
- Heat-Related Illnesses
- Heat Cramps
- Heat Exhaustion
- Heat Stroke
- Cold-Related Illnesses
- Frostbite & Frostnip
- Non-Freezing Cold Injury (NFCI)
- Hypothermia
- Stages of Hypothermia
- Application of a Hypothermia Wrap
- Frozen Cornea
- Snow Blindness
- Freezing Skin to Metal Objects
- Water-Related Illnesses
- Cold-Water Immersion
- Self-Rescues
- Rescuing Another Person from Water or Ice
- Drowning
- High-Altitude Illness
- SCUBA-Related Illness
- Lightning Injuries
- Signs & Symptoms of Frostnip
- Signs & Symptoms of Frostbite
- First Aid for Frostbite and Frostnip
- Signs & Symptoms of Mild Hypothermia
- Signs & Symptoms of Moderate Hypothermia
- Signs & Symptoms of Severe Hypothermia
- First Aid for Hypothermia
- Signs & Symptoms of Heat Cramps
- Signs & Symptoms of Heat Exhaustion
- Signs & Symptoms of Heat Stroke
- First Aid for Hyperthermia
- Poisonous Plants
- Hogsweed
- Devil's Club
- Poison Ivy
- Poison Oak
- First Aid for plant exposure
- Animal Bites
- Rabies
- First Aid for Animal Bites
- Snake Bites
- Rattlesnakes
- First Aid for snake bites
- Jellyfish Stings
- Tick Bites
- Lyme Disease
- First Aid for Tick Bites
- Wildlife-Related Injuries and Illnesses
- Animal Bites
- Wild Animal Safety
- Hantavirus
- Animal Stings
- Stings from Marine Life
- Jellyfish Stings
- Insect Stings
- Leeches
- Spider Bites
- Regional Awareness & Preparation
Wilderness First Aid for Extended Care
.jpg)
One of the most significant, and often underestimated, responsibilities associated with acting as a Wilderness First Aid responder is providing extended and ongoing medical care for a patient in remote areas. Unlike medical emergencies in urban areas where paramedics, ambulances and medical centers are readily available, a Wilderness First Aid responder may be the most qualified available for an extended time period. Depending on the location of the injury, trip parameters, group dynamics transport options and weather patterns, it make be hours, days, or even weeks before the patient can be delivered to definitive medical care. In the meantime, a Wilderness First Aid responder will need to do everything reasonably possible to prevent injuries or illnesses from worsening, causing permanent disability or even death. It's always important to keep in mind that the circumstances and nature of the injury or illness could outperform the training and resources available to the Wilderness First Aid responder and a negative outcome may be unavoidable despite best efforts.
Activities and interventions that would be considered routine in normal circumstances can become complicated, time consuming and even risky in a remote outdoor location. A patient's toileting needs will not diminish just because they are unable to stand or walk, but soiled clothing and bedding will not only increase the chances of infection and medical complications, but also potentially attract local pests and wildlife endangering the entire camp. Minor wounds can lead to life-threatening infection and cause septic shock if left unattended, so daily inpection and cleaning of the affected tissues is extremely important in an extended care scenario. In many cases, a Wilderness First Aid responder will bring prescription antibiotics in the medical kit, after obtaining permission and instructions from a qualified physician or medical director.
Depending on the planned duration of the trip and how far into it the medical emergency occured, it may become necessary to improvise overnight shelter, make a fire, ration food and water supplies, and maximize insulation to keep the patient warm, nourished, and hydrated. The ability to maintain regular sleep patterns in a significant factor in the overall wellness and response capacity of the group, as well as patient stabilization and recovery. The ongoing health and wellness of Wilderness First Aid responder is important as well, so it may be necessary to delegate some of your duties to another member of the group. Extended remote medical care principles covered in your Canadian Red Cross Wilderness First Aid course and materials include...
- Shelter
- Fire
- Food
- Oxygen
- Water
- Water Purification Techniques
- Types of Shelter
- Site Selection for Shelters
- Monitoring an Ill or Injured Person
- Body Positions and Movement
- Personal Hygeine
- Toileting Care
- Rest
- Extended Wound Care
- Improvised Sterilization Techniques
- Abscess Draining
- Pain Management
- Psychological Care
- Documentation
Wilderness First Aid for Emergency Transport
.jpg)
When a medical emergency occurs in a remote or outdoor setting, the intial group response efforts are generally focused on dealing with immediate life-threatening conditions, assembling or improvising appropriate shelters, and then settling into ongoing patient care and comfort. Eventually, however a decision needs to be made regarding the best strategy to get the patient to definitive medical care and/or long term recovery facilities. There are many factors to consider in the transport decision including the urgency of the patient's condition, on location communication options, distance and terrain to the nearest roadway, watercraft or airstrip, trip supplies, group capacity, and weather conditions.
The available options will largely depend on the resources identified and secured during the pre-trip planning stage. If you have a two-way communciation device capable of transmitting your location and needs, it may be possible for someone at home to arrange for emergency transport and medical assistance. If communications are not possible where you are, you may need to consider sending a portion of the group to an area with better signal or even back to the nearest town to send for help. In both cases it's extremely important that your exact current location is accurately documented and communicated whether that includes a GPS coordinate or route plotting on a paper map.
Although helicopters are generally considered the fastest and safest way to evacuate someone from the wilderness, the terrain at your current location may not accommodate a landing or extraction. If that's the case you may need to consider moving the patient to another, more rescue friendly area. Transporting a patient in a canoe or kayak is much less physically strenuous than overland extrication, but you need to consider the likelyhood and potential consequences of the craft taking on water or capsizing. If the patient is incapable of swimming or remaining afloat they would likely drown in such a scenario, and possibly place the rest of the group in danger. Carrying a patient in an improvised litter might be the only tranpsort option available, but you'll need to realistically consider the physical limitations of the group compared to the distance terrain being travelled. A trail that is relatively easy during dry, well lit conditions may become dangerous or impassable during periods of darkness, heavy rain or snowfall. In all cases the overall well being of the entire group must be considered, as well as the urgent medical needs of the patient. Emergency rescue, evacuation and care principles covered in your Canadian Red Cross Wilderness First Aid course and materials include...
- Transportation Planning
- Sleds
- Boats
- Helicopters
- How to Lead
- Stretchers
- Improvised Stretchers
- Moving the Person to Safety vs. Moving the Person to Transport Option
- Patient Drags
- Patient Lifts
- Patient Carries
- Patient Care During Transport
- Getting Help
- Signalling
- Communication Devices
- Geolocation Devices
- Navigation
- Route Planning
- Arranging Transport
- Activating Professional Rescue
tel: 778-724-9054 email: training@mediprofirstaid.com
We recognize and respectfully acknowledge that we operate on the traditional and unceded territory of the Syilx Okanagan and Secwepemc peoples.

.png)
.png)
.png)
As a participant in a Canadian Red Cross Wilderness First Responder course, you will need to work with and show respectful behaviour towards all of your classmates. Regardless of any personal, philosophical, religious or political differences, you must support each other's learning throughout the course.
Respect is particularly important when learning, practicing or performing skills that involve physical contact with another participant. Physical contact is an unavoidable component of many core First Aid and CPR skills, so participants must be as respectful and professional as possible during these segments.
Each participant will bring their own unique experiences, backgrounds and perspectives to your Wilderness First Responder course, which will make the course more interesting and relevant for everyone, provided mutual respect is consistently demonstrated. Language or actions which impinge on every participants' right to a physically and psycologically safe learning learning environment will not be tolerated, and will result in expulsion from the program. You are not expected to agree with every aspect of your classmates' lifestyles and opinions, however you are expected to demonstrate respectful behaviour towards each other at all times.