Emergency Medical Responder
.png)
Emergency Medical Responder Course Summary
| EMR Course Registration |
| EMR Course Overview |
| EMR Course Preparation |
| EMR Course Skills |
Medi-Pro Response Solution's Canadian Red Cross Emergency Medical Responder courses are intensive, interactive and learner centered programs which prepare you and provide you with BC EMALB EMR Licensing eligibility. You will learn and practice a systematic but flexible approach to patient assessment, advanced medical interventions, pharmacology, and clinical decision making in a professional emergency medical response capacity.
The skills taught and principles introduced are nationally recognized for scientific, evidence-based credibility, with a strong emphasis on provincially relevant BCEHS Clinical Practice Guidelines and BC EMALB Licensing Exam requirements.
EMR Certification
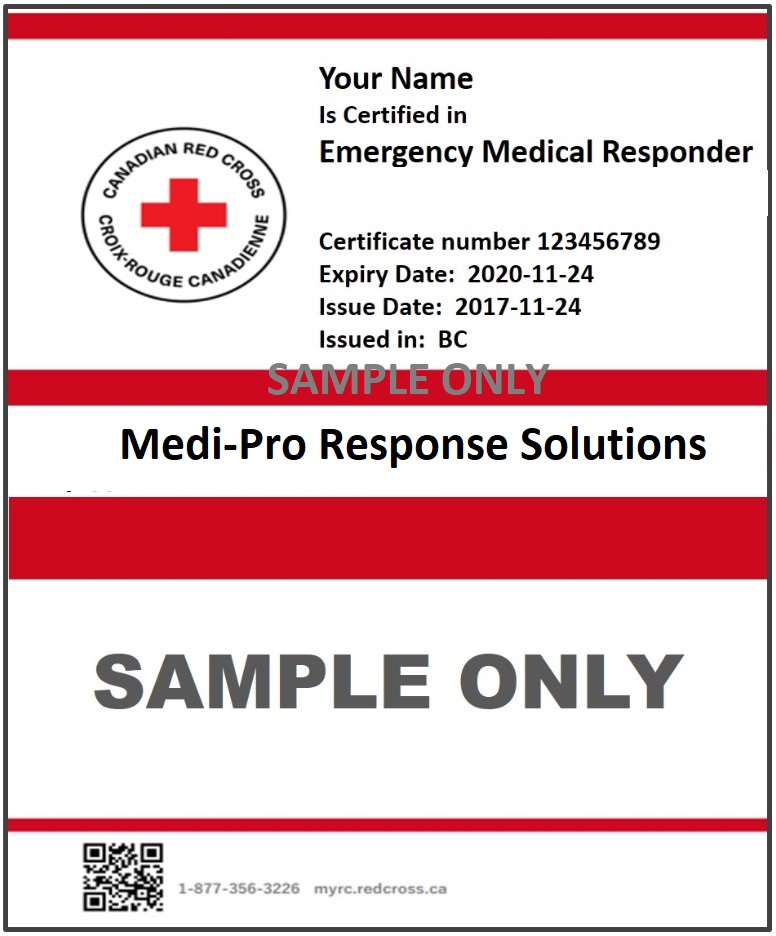
Upon successful completion of the Emergency Medical Responder program you will receive an EMR certificate, as issued through the Canadian Red Cross, valid for 3 years. You will also receive a separate Basic Life Support (BLS) certificate valid for 1 year. Canadian Red Cross certificates are generated and issued electronically through the national MyRC database, and provided by email within 10 business days of completion of all course and examination requirements. More...
EMALB Licensing
You will be eligible to engage and complete the British Columbia Emergency Medical Assistants Licensing Board (BC EMALB) Emergency Medical Responder Licensing exams for one year after receiving your Canadian Red Cross Emergency Medical Responder certificate. BC EMALB EMR Licensing exams include an online Written EMR Knowledge exam, an online Written Jurisprudence exam and two scenario-based Practical exams (one Trauma based and one Medical Emergency based). You will need to directly communicate with BC EMALB yourself to start, schedule and complete the EMR Licensing process. More...
BCEHS Scope of Practice
Medi-Pro's Canadian Red Cross Emergency Medical Responder courses include the most current, 2024, BCEHS Scope of Practice including Schedule 1 and Schedule 2 of the Emergency Health Services Act for the EMR licence level. These expanded EMR Scope of Practice skills include Intramuscular/Subcutaneous Glucagon Administration, Wound Packing, Anti-Clotting Agents, Inhaled Analgesics such as Methoxyfluorane (Penthrox), Weight-Based Administration of Epinephrine by Intra-Muscular Injection, and Administration of Salbutamol (Ventolin) by Nebulizing Mask or Metered Dose Inhaler. More...
Occupational First Aid Certification
As of November 1st, 2024 WorkSafe BC has ceased maintaining and supporting its Occupational First Aid (OFA) programs and instead recognizes other first aid certifications for either Basic, Intermediate, or Advanced First Aid attendant qualification requirements. More...
EMR, EMR Bridge & EMR Recertification
EMR courses are typically delivered over 130 hours with full-day classroom sessions. If you currently hold a valid, un-expired OFA 3 certificate or First Responder certificate you are eligible to participate in a shortened EMR Bridge course (100 hours). If you currently hold a valid, un-expired EMR certificate you are eligible participate in a shortened EMR Recertification course (100 hours). There is an online based EMR study guide, which participants are encouraged to complete prior to or during the EMR course itself. There is also a post-course online eLearning module covering the newly expanded BCEHS scope of practice. The time required to complete the eLearning Modules and the Study Guide will vary, however you should anticipate and allocate at least 12 hours for pre-course activities. More...
Emergency Medical Responder Course Overview
Review the information in this section to make sure that Emergency Medical Responder will meet your training and certification needs, and give yourself the tools to arrive fully prepared for success and enjoyment in your EMR course. Emergency Medical Responder certification training, and the corresponding BC EMALB Licensing process require a significant investment of time and effort, so you should make sure you know what you're getting, and what you're getting into.
What You Get
.jpg)
What's included with your Kelowna Canadian Red Cross Emergency Medical Responder course and registration fees?
- Eligibility for BC EMALB Emergency Medical Responder Licensing evaluations (must be completed within one year of EMR certification).
- The most current and up to date BCEHS Scope of Practice.
- Canadian Red Cross Emergency Medical Responder (EMR) certification (valid for 3 years).
- Canadian Red Cross Basic Life Support (BLS) certification (valid for 1 year).
- Canadian Red Cross Emergency Care for Professional Responders reference manual (online access to the PDF version is included with your registration and you have the option to purchase a printed take-home copy).
- Online EMR Study Guide.
- Access to Medi-Pro's extensive library of online resources and support materials.
BC EMALB Licensing
.gif)
Canadian Red Cross Emergency Medical Responder course completion provides you with eligibility for the BC Emergency Medical Assistant's Licensing Board (EMALB) EMR Licensure including the most current, 2024, BCEHS Scope of Practice for Schedule 1 and Schedule 2 of the Emergency Health Services Act.
These expanded EMR Scope of Practice skills include Intramuscular/Subcutaneous Glucagon Administration, Wound Packing, Anti-Clotting Agents, Inhaled Analgesics such as Methoxyfluorane (Penthrox), Weight-Based Administration of Epinephrine by Intra-Muscular Injection, and Administration of Salbutamol (Ventolin) by Nebulizing Mask or Metered Dose Inhaler.
You will need to arrange and complete your BC EMALB EMR Licensing Evaluations within one year of obtaining your EMR certification. As your EMR course will include the most current skills for BCEHS Schedule 1 and Schedule 2 of the Emergency Medical Assistant's Regulation, you will not need to conduct further training after you obtain your license and you will be eligible to provide the current Scope of Practice. BC EMALB EMR Licensing Evaluations are administered and managed through BC EMALB directly. EMR Licensing Evaluations include an online Written Exam, an online Jurisprudence Exam, and two practical Scenario Evaluations (one Medical Emergency based and one Major Traumatic Injury based).
Click here for more information about the BC EMALB EMR Licensing Evaluations and requirements.
Canadian Red Cross EMR Certification
Our Canadian Red Cross Emergency Medical Responder programs are Nationally recognized for up to date protocols, and meet the most current BCEHS Clinical Practice Guidelines, and BC EMALB Licensing exam requirements.
You'll learn and practice advanced emergency medical assessment and interventions which will help you make safe decisions in any emergency, and provide professional medical care to your patients.
Your Canadian Red Cross EMR certificate, awarded to you upon completion of your Kelowna EMR course and valid for 3 years, will indicate Canadian Red Cross Emergency Medical Responder certification, which is a prerequisite for BC EMALB EMR Licensure. You will also receive a Canadian Red Cross Basic Life Support (BLS) certificate, valid for one year.
Canadian Red Cross certificates are generated and issued electronically through the national MyRC database, and provided by email within 10 business days of completion of all course and examination requirements. More than just a certificate, you'll have the confidence to act, and Be the Difference in your community.
WorkSafe OFA 3 Certification
.gif)
As of November 1st, 2024 WorkSafe BC has discontinued support and maintenance of it's in-house Occupational First Aid programs. These include Occupational First Aid level 1 (OFA 1) certification, Occupational First Aid level 1 (OFA 2) certification, and Occupational First Aid level 3 (OFA 3) certification. WorkSafe BC has also updated their workplace First Aid Attendent qualification requirements to reflect these changes and has designated three general categories of First Aid training including Basic First Aid certifications, Intermediate First Aid certifications, and Advanced First Aid certifications.
Workplaces which would have previously required Occupational First Aid level 1 (OFA 1) certified attendants now require first aid attendants certified in Basic First Aid. Canadian Red Cross Emergency First Aid courses and Standard First Aid courses, both of which include CPR-AED level C, have been granted preliminary approval for meeting WorkSafe BCs Basic workplace First Aid attendant qualifications.
Workplaces which would have previously required Occupational First Aid level 2 (OFA 2) certified attendants now require first aid attendants certified in Intermediate First Aid. WorkSafe BC has not yet explicitly identified Standard First Aid certification and First Responder certification as meeting their Intermediate First Aid certification requirements, so you should check with your employer or WorkSafe BC directly to ensure you are completing the level of training they require.
Workplaces which would have previously required Occupational First Aid level 3 (OFA 3) certified attendants now require first aid attendants certified in Advanced First Aid. WorkSafe BC has not yet explicitly identified First Responder certification, Emergency Medical Responder (EMR) certification, or Advanced First Aid (AFA) certification as meeting their Advanced First Aid attendant training requirements, so you should check with WorkSafe BC directly to ensure you are completing the level of training they require. Click here for more information about WorkSafe BC's Occupational First Aid attendant certification policies and requirements as they related to Emergency Medical Responder training, certification, and licensure.
Basic Life Support
.png)
In addition to your 3 year Emergency Medical Responder (EMR) certificate, you will also receive a separate Basic Life Support (BLS) certificate which is valid for 1 year. Basic Life Support is essentially a high performance, "pit-crew" approach to Cardiopulmonary Resuscitation (CPR) and Automated External Defibrillation (AED) in a professional medical responder environment.
Basic Life Support principles form an integral part of your overall Emergency Medical Responder training, and are also considered a standalone, portable skill set that can be transferred to work with any high performance team performing CPR in a clinical setting. Your Emergency Medical Responder certification includes BLS protocols, and remains valid for 3 years, however the separate Basic Life Support certificate issued at the same time will only remain valid for 1 year. If you require a valid BLS certificate, you will need to complete a standalone BLS Recertification course yearly, but your EMR certificate will remain valid for the full 3 year term regardless of whether or not you specifically renew the BLS certificate.
There is an emphasis on the specific Basic Life Support protocols stipulated and outlined by the local authorities having jurisdiction (AHJ) in British Columbia including the Emergency Medical Assistant's Licensing Branch (EMALB) examination guidelines, BC Emergency Health Services (BCEHS) Clinical Practice Guidelines, and BC Ambulance Service (BCAS) response guidelines. Basic Life Support skills, tools and principles covered in your Emergency Medical Responder course include...
- Team based approach to CPR & AED with multiple rescuers/agencies on scene
- Variable Compression to Ventilation ratios for patients in different age groups
- Adult patients aged 9 and up (30:2/10:1/CCC)
- Child patients aged 1 to 9 (15:2)
- Infant patients under 1 year old (15:2)
- Neonatal patients under 28 days old (3:1)
- Bag-Valve-Mask (BVM)
- Oxygen Therapy
- Oropharyngeal Airways
- Nasopharyngeal Airways
- Automated External Defibrillators
- CPR in Transport/Treatable CPR
Where to go
.png)
Our Canadian Red Cross Emergency Medical Responder courses are provided in multiple classroom locations in Kelowna, Vancouver, the Lower Mainland and throughout British Columbia. Most EMR courses in the Okanagan area are conducted in our West Kelowna classroom at 2011 Daimler Drive. Click here for directions, maps and public transit options.
By request, we can schedule private courses for your group at specific location of your choosing. The location and directions for your particular Emergency Medical Responder course will be indicated during the booking process, and included in the confirmation email you will receive upon completing registration.
- Make sure the EMR course you are registering for is in a location that works for you.
- Our booking platform may show EMR courses at different geographic regions on different course dates.
- Check your confirmation email to ensure that the course location indicated is in the region you expected.
- The link in your confirmation email will incude directions, but you should verify your intended route of travel ahead of time.
- Allow ample time for traffic and unanticipated delays to ensure you arrive at your classroom in time for your scheduled course sessions.
EMR Course Schedule
.jpg)
Get the most out of your Kelowna Emergency Medical Responder course by familiarizing yourself with the EMR course content, schedule, and classroom session structure. Your Canadian Red Cross EMR course in Kelowna or Vancouver, BC, with EMALB Licensing eligibility, is 130 hours structured into full-day classroom sessions. Kelowna and Vancouver EMR courses are generally scheduled mid-week (Monday to Friday, Monday to Friday, Monday to Wednesday) over two and a half consecutive weeks, concluding mid-week on the third Wednesday. EMR Bridge courses and EMR Recertification courses are generally scheduled over two consecutive weeks (Monday to Friday, Monday to Friday).
EMR concepts, principles, and skills are introduced in a simplified context and logical sequence. The Emergency Medical Responder course starts with basic drills, and builds towards more complex scenarios with an emphasis on clinical decision making as participant skill levels and confidence improve. Stand-alone skill components are introduced and reinforced, then integrated into realistic situations and circumstances. Intensity, workload and student responsibilities increase as the EMR course progresses, with developing emphasis on clinical decision making abilities and adaptive skill application.
Each EMR course session includes two short breaks and one longer lunch break throughout the day. Access to locals stores or restaurants may be limited, so you should arrive at each session with enough food and water/drinks to keep you nourished and hydrated the entire day. Your Canadian Red Cross EMR written exam, and two EMR practical scenario evaluations will take place throughout the final classroom sessions.
The last few sessions of your Emergency Medical Responder course will focus on reviewing, practicing, and expanding on all the topics, skills and principles covered in previous the sessions. Performing a skill or reading a text passage once will not prepare you for success. In order to be successful in your final evaluations, EMALB Licensing Exams and in providing patient care as a professional responder you need to have a reflexive familiarity, born of repetition and feedback, with all aspects of your EMR training. The more you review the key concepts and practice the foundational skills, the more you can focus on problem solving the unique challenges of each patient and circumstance.
These final EMR course sessions will be your opportunity to identify areas that you feel less comfortable with, and ask your Instructor to work with you on them to improve your confidence and skill levels. Most of the time spent in the classroom at this point will be dedicated to full simulation scenarios, and you can request specific topics or versions of these scenarios based on your own evaluation of your readiness and needs as a learner. You may feel comfortable performing CPR as a hands-on skill, but need more clarification on the criteria for Treatable CPR and CPR in Transport. You may have the Indications and Contraindications for Entonox memorized, but want to practice the hands-on application of a Traction Splint. You will also have the opportunity to practice established skills in more complex scenarios and challenging circumstances to more accurately reflect real-life applications. EMR principles, skills and concepts reviewed, practiced and reinforced throughout the review and practice sessions of your Canadian Red Cross Emergency Medical Responder course include...
- EMR Assessment Model review
- Glasgow Coma Scale review
- NEXUS Spinal Motion Restriction criteria review
- FAST VAN Stroke Assessment review
- Manual SMR stabilization practice
- Nitroglycerin Indications and Contraindications review
- ASA Indications and Contraindications review
- Naloxone (Narcan) Inidications and Contraindications review
- Entonox Indications and Contraindications review
- Glucogel Indications and Contraindications review
- Glucagon Indications and Contraindications review
- Epinephrine Indications and Contraindications review
- Salbutamol (Ventolin) Indications and Contraindications review
- Traction Splint application practice
- Respiratory Distress management practice
- Respiratory Arrest management practice
- Verbal and written patient care hand-over practice
- Treatable CPR review
- Pit Crew CPR-AED review
- CPR with Airway Obstruction review
- Review & Practice Medical and Trauma based scenarios
EMR Exams & Remediation
.jpg)
The final sessions of your Emergency Medical Responder course will include your formal Canadian Red Cross EMR Certification exams. Successful completion of our Canadian Red Cross Emergency Medical Responder course includes meeting minimum performance requirements in the Written Evaluation and two Practical Scenario Evaluations. The Canadian Red Cross EMR written exam involves answering 100 multiple choice questions in a proctored and timed environment. One practical scenario exam will emphasize providing patient care for a medical condition such as myocardial infarction, hypoglycemia, anaphylaxis, or congestive heart failure. The other practical scenario exam will emphasize providing patient care for a traumatic physical injury such as femur fracture, spinal cord injury, concussion, or tension pneumothorax.
The minimum score required for successful completion of the Canadian Red Cross Emergency Medical Responder written knowledge evaluation is 75%, which coincides with local BC EMALB evaluation practices. The practical scenarios evaluations follow a more subjective grading process involving minor, major, or critical point deductions assigned to individual patient care deficits, with an overall outcome of successful or unsuccessful based on several coinciding factors. You will be permitted up to two attempts at the written knowledge evaluation, and the practical scenario evaluations. If you are successful on your first attempt at each evaluation component, you will be marked successful for that specific component regardless of your performance in any subsequent components.
Not everyone is successful in receiving EMR certification on their first attempt. In the event that you are unsuccessful in your first attempts at the formal EMR Certification evaluations, you will be afforded a second opportunity to demonstrate the required skills and knowledge. Your EMR Instructor will work with you and Medi-Pro to formulate a remediation plan that will maximize your chances for success as a professional medical responder. Most of the time, this will involve scheduling a re-testing session near the end of our next scheduled EMR course, as well as the opportunity to participate in some practice and review beforehand. Every remediation plan will be unique to each participant's particular needs, so the process may be different for each individual. We want you to be successful in your initial EMR certification, BC EMALB Licensing process, and in your career as a professional medical responder.
EMR principles, skills and concepts reviewed, practiced and reinforced throughout the formal evaluation portion of your Canadian Red Cross Emergency Medical Responder course include...
- Final Canadian Red Cross Emergency Medical Responder Written Exam
- Trauma-based Canadian Red Cross Practical Scenario Evaluation
- Medical-based Canadaian Red Cross EMR Practical Scenario Evaluation
- Canadian Red Cross EMR Certification process
- BC EMALB EMR Licensing Evaluation procedures
- Emergency Medical Responder next steps
Frequently Asked Questions
.jpg)
Frequently Asked Questions about Canadian Red Cross Emergency Medical Responder certification courses in Kelowna and Vancouver BC. Take a look through the Q & A topics listed below, to find answers to your Emergency Medical Responder course questions. If you don't see the answers to your questions in this FAQ section, you may still find the information you're looking for in the other sections of this page, including Emergency Medical Responder Overview, Emergency Medical Responder Resources, and Emergency Medical Responder Course Skills.
Of course, Medi-Pro First Aid is happy to answer all your questions if you choose to contact us directly through our Contact Us form, by email (training@mediprofirstaid.com), or over the phone (778-724-9054). We do our best to respond to all enquiries as quickly as possible during normal business hours from 9am to 5pm, Monday-Friday.
Q. Will my Emergency Medical Responder course include the most current Scope Practice?
Yes. As of March 2024 our Canadian Red Cross EMR courses include the current (2024) scope of practice as required by BC EMALB and outlined in Schedule 1 and Schedule 2 of the Emergency Health Services Act. Upon obtaining your BC EMALB Emergency Medical Responder Licence you will be immediately eligible to have the relevant scope of practice restrictions removed and you will be able to provide patient care at the current scope.
Q. When will I get my EMR Certificate?
Canadian Red Cross Emergency Medical Responder certificates are generated on the national MyRC course management platform and provided to Emergency Medical Responder course participants electronically, in PDF format. Upon successful completion of your Emergency Medical Responder course, Medi-Pro will upload and process your certification, and you will recieve your EMR certificate by email. Medi-Pro administration do their best to ensure this process is generally completed within 48 hours of course completion, but it in some circumstances it can take up to 10 business days. If you require immediate proof of Emergency Medical Responder course completion, your Instructor can provide you with a temporary certificate before you leave the classroom. However it is up to each individual employer/regulatory agency to decide whether or not they accept temporary certificates. It is usually simplest to just forward your official Emergency Medical Responder certificate and/or your Basic Life Support certificate as soon as you receive it.
Q. Can I get a refund if I cancel my Emergency Medical Responder course registration?
Medi-Pro's baseline policy is no refunds for last minute cancellations. However, we will do our best to work with you if circumstances beyond your control make it impossible for you to attend your scheduled course. In most cases, we can find an alternative course date for you and just move your existing registration to the new date. Depending on circumstances, and the number of previous cancellations, there may be a small re-booking charge, but we're compassionate people who understand that life can be messy.
Q. How long is an Emergency Medical Responder course?
In order to meet BCEHS requirements for EMALB Licensure, the minimum classroom time required for a Canadian Red Cross Emergency Medical Responder course is 120 hours in British Columbia. Medi-Pro generally schedules Emergency Medical Responder courses over 2.5 weeks of full day classroom sessions Mon-Fri, Mon-Fri and Mon-Wed. This allows you enough time to not only learn EMR principles for the first time but also perform multiple repetitions of the skills and scenarios and build lasting confidence and leave you prepared for success in your EMALB Licensing exams. If your group requires a different timeframe, such as multiple weekends or a specific day of the week broken up across multiple weeks, you can make arrangements with Medi-Pro for a private booking that works for your group's scheduling needs.
Q. Is this a WorkSafe BC Occupational First Aid (OFA) course?
As of November 1st, 2024 WorkSafe BC has discontinued support and maintenance of it's in-house Occupational First Aid programs. These include Occupational First Aid level 1 (OFA 1) certification, Occupational First Aid level 1 (OFA 2) certification, and Occupational First Aid level 3 (OFA 3) certification. WorkSafe BC has also updated their workplace First Aid Attendent qualification requirements to reflect these changes and has designated three general categories of First Aid training including Basic First Aid certifications, Intermediate First Aid certifications, and Advanced First Aid certifications.
Q. Is there an age requirement for Emergency Medical Responder courses?
The Canadian Red Cross does not have any age requirements to complete an Emergency Medical Repsonder course or to receive EMR certification. Participants of any age are welcomed in our Emergency Medical Responder courses, provided they are capable and willing to actively participate throughout the entire course. Of course, there are some considerations that might make it inappropriate for a very young participant, but there is no minimum age specification.
BC EMALB stipulates that you must be at least 19 years old to provide emergency medical service as a licensed practitioner in BC. You can obtain and hold a "Restricted" EMALB licence from 16-18 which means you can only provide emergency medical service under the direct supervision of an unrestricted (at least 19 years old) EMALB Licence holder. A restricted licence automatically becomes unrestricted when the licence holder turns 19.
Q. Can I renew/recertify my old Emergency Medical Responder certificate?
If you hold a current and valid Emergency Medical Responder certificate from Canadian Red Cross, St. John Ambulance or another recognized provider, you qualify to complete a shortened Emergency Medical Responder Recertification course. If your most recent EMR certificate has already expired, you will need to re-complete the full Emergency Medical Responder course to obtain a new EMR certificate.
Q. I can't find my EMR Certificate. How can I get a replacement?
If you took your last Emergency Medical Responder course with Medi-Pro Response Solutions or Frontline First Aid, we likely have a record of your certificate on file. Just let us know that you need a replacement copy and we'll send it out to you by email. Make sure to tell us if your email address has changed since your last Emergency Medical Responder course registration, or if you need the copy sent to a different email.
Q. Where do Emergency Medical Responder guidelines come from?
The International Liason Committee on Resuscitation (ILCOR), and the corresponding Consensus on Science and Treatment Recommendations (CoSTR) task force groups constantly review and evaluate current Professional Medical Responder and Basic Life Support practices from data collected around the globe. ICLOR and CoSTR periodically produce documents which summarize their most recent findings, as well recommendations on what current emgergency paramedical practices should be continued, which should be changed, and what new practices should be adopted. Based on the findings in these documents, as well as other scientifically credible sources, individual Emergency Medical Responder and Paramedic training providers such as the Canadian Red Cross produce their own evidence-based guidelines and educational delivery models.
In British Columbia, the paramedic profession is governed and regulated by BC Emergency Health Services (BCEHS) and the BC Emergency Medical Assistant's Licensing Board (EMALB). As such your Emergency Medical Responder course will include many skills and protocols which are specific to British Columbia as dictated by BCEHS and EMALB which are updated frequently.
Q. Should I take an Emergency Medical Responder course?
Emergency Medical Responder is the entry level certification required to provide professional pre-hospital care within the Paramedic Association of Canada (PAC) scope of training. Emergency Medical Responder training is also one of the prerequisites for entrance into the British Columbia Paramedic Academy's Primary Care Paramedic (PCP) program, which can lead to employment opportunities with the BC Ambulance Service (BCAS) as a career Paramedic.
Many Fire Departments and Fire-Rescue Agencies in BC and Alberta are moving toward Emergency Medical Responder as their baseline medical training and response level for the hiring of new fire fighter recruits. Anyone who is looking at starting or furthering their career as a professional medical responder should consider an EMR training program and the corresponding BC EMALB Licensing process.
- Paramedics
- Fire Fighters
- Care Aides
- Nurses
- Occupational First Aid Attendants
- Remote Oilfield Medics
- Search and Rescue workers
- Ski Patrollers
- Care Providers
- Harm Reduction workers
You should always confirm specific course and certification requirements with your employer, educational institution or governing body before making your course selection. Medi-Pro First Aid can provide you with best practice recommendations based on industry standards, but cannot make a blanket guarantee that any particular First Aid/Medical Responder course will meet your individual requirements.
Q. What is Hands-Only CPR?
The baseline performance of bystander CPR includes continuous cycles of chest compressions combined with alternating ventilations/rescue breaths. The chest compressions pump blood from the heart and circulate it to vital organs. The rescue breaths put oxygen back into the lungs and bloodstream so that the blood being circulated is keeping cells alive. Ideally, an AED should be used as soon as possible as well.
Hands-Only CPR (also known a Compresssions-Only CPR) is an alternative which takes into account that a bystander may not feel safe or comfortable performing the rescue breathing component. Performing the chest compressions continuously, without providing rescue breaths, can still produce a positive outcome without the real or perceived risks associated with rescue breathing. Although not as statistically effective as traditional CPR, the application of Hands-Only CPR has been proven vastly superior to doing nothing, and can help ensure the patient is still viable when emergency crews arrive to perform more advanced procedures.
Emergency Medical Responder Course Preparation
You will maximize your opportunities for success enjoyment through your Canadian Red Cross Emergency Medical Responder course in Kelowna and Vancouver, BC (and the subsequent BC EMALB EMR Licensing Evaluations) if you review the basic expectations and arrive fully prepared, with your EMR Study Guide completed.
The more familiar you are with the online resources, educational supplements, printed text books, and EMR support materials at your disposal, the more likely you are to enjoy your EMR course and be successful in obtaining EMR certification and licensure.
.jpg)
Access and complete our EMR Study Guide to help prepare you for your Emergency Medical Responder course in Kelowna and Vancouver, BC. The EMR Study Guide has been developed to help prepare you for success and enjoyment in your BC Emergency Medical Responder course.
There are two significant sources of information and EMR protocols for Emergency Medical Responders training and practicing in British Columbia. The Canadian Red Cross provides you with a Nationally recognized EMR Program and Certification, following the content in the Emergency Care for Professional Responders reference manual. BC EMALB has jurisdiction over Provincial EMR Licensing in BC, and has a few BC specific protocols, based on the EMALB Examination Guidelines and BCEHS Treatment Guidelines, that differ slightly from the national Canadian Red Cross program.
Completing the EMR Study Guide before starting your Emergency Medical Responder course will help make sure you arrive familiar with the information and resources available to you. Your Emergency Medical Responder course classroom sessions will center primarily on physical skills and hands-on practice and application, so the Study Guide will also help ensure that you have the background information and theory needed.
EMR Study Guide Sections:
- Section A: Text Book Corrections
- Section B: Certification and Licensing
- Section C: BC EMALB Jurisprudence
- Section D: EMALB Examination Guidelines
- Section 1: The Professional Responder
- Section 2: Responding to the Call
- Section 3: Infection Prevention and Control
- Section 4: Anatomy and Physiology
- Section 5: Assessment
- Section 6: Airway Management and Respiratory Emergencies
- Section 7: Circluatory Emergencies
- Section 8: Shock
- Section 9: Hemorrhage and Soft Tissue Trauma
- Section 10: Musculoskeletal Injuries
- Section 11: Chest, Abdominal and Pelvic Injuries
- Section 12: Head and Spinal Injuries
- Section 13: Acute and Chronic Illness
- Section 14: Poisoning
- Section 15: Environmental Illnesses
- Section 16: Pregnancy, Labour, and Delivery
- Section 17: Special Populations
- Section 18: Crisis Intervention
- Section 19: Reaching, Lifting, and Extricating Patients
- Section 20: Transportation
- Section 21: Multiple Casualty Incidents
- Section 22: Pharmacology
- Section 23: Marine Environment
- Section 24: Workplace
Emergency Care for Professional Responders
Canadian Red Cross Emergency Care for Professional Responders reference manual. Utilized by Emergency Medical Responder course participants in Kelowna and Vancouver, BC.
The vast majority of the emergency medical skills, principles, guidelines and metrics you will learn and practice in your Canadian Red Cross Emergency Medical Responder course are based on the Emergency Care for Professional Responders text book, which follows the Paramedic Association of Canada's (PAC) National Occupational Competency Profiles (NOCP).
The Canadian Red Cross Emergency Care for Professional Responders
reference manual is a 453 page, full-color text book with a soft red and white cover. Emergency Care for Professional Responders is available as a downloadable PDF, and in a printed edition. Electronic access to the PDF version is included with your Emergency Medical Responder course registration, and you have the option to purchase a take-home printed copy as well.
The Canadian Red Cross Emergency Care for Professional Responders reference manual can also be purchased by anyone with an interest in the most current and scientifically valid evidence-based Emergency Medical Care practices in Canada.
Emergency Care Manual Contents:
- Professional Responder Training Levels
- Preceptorship
- Medical Oversight
- Communicating with the Medical Director
- Professional Responder Responsibilities
- Interpersonal Communication
- Self-Care
- Critical Incident Stress and Post-Traumatic Stress Disorder
- Legal and Ethical Issues
- Duty to Act
- Scope of Practice
- Abuse and Neglect
- Consent
- Refusal of Care
- Transfer of Care
- Documentation
- Communication
- Medical Terminology
- Preparing for the Emergency
- Response
- Equipment
- Plan of Action
- Communications
- Training
- Psychological Preparation
- Managing Hazards at the Emergency Scene
- Personal Safety
- Safety of Others
- Special Emergency Scenes
- Specific Scene Hazards
3. Infection Prevention and Control
- How Infections Occur
- Disease-Causing Pathogens
- How Diseases are Transmitted
- Epidemics and Pandemics
- Diseases that Cause Concern
- Immunization
- Preventing Disease Transmission
- Personal Hygeine
- Personal Protective Equipment (PPE)
- Engineering and Work Practice Controls
- Cleaning and Disinfecting Equipment
- Spill Management
- Exposure Control Plans
- If an Exposure Occurs
- Anatomical Terminology
- Body Cavities
- Body Systems
- The Cell
- Respiratory System
- Circulatory System
- Lymphatic System
- Immunological System
- Nervous System
- Musculoskeletal System
- Integumentary System
- Endocrine System
- Digestive System
- Genitourinary System
- Interrelationships of Body Systems
- How Injuries Occur
- Scene Assessment
- Primary Assessment
- Reassessment
- Secondary Assessment
- Treatment/Interventions
- Documentation of Findings
- Ongoing Assessment
6. Airway Management and Respiratory Emergencies
- Respiratory Pathophysiology
- Airway Obstruction
- Respiratory Conditions
- Assisted Ventilation
- Resuscitation Devices
- Resuscitation Masks
- Bag-Valve-Mask (BVM) Rescusitators
- Supplemental Oxygen
- Airway Adjuncts
- Oropharyngeal Airways
- Nasopharyngeal Airways
- Supraglottic Airways
- Suction
- Care for Respiratory Distress
- Care for Respiratory Arrest
- Cardiovascular Disease
- Angina
- Myocardial Infarction (MI)
- Congestive Heart Failure
- Cardiac Arrest
- Cardiopulmonary Resuscitation
- Compressions
- Team Approach
- Using a Defibrillator
- Special Resusciation Situations
- Post-Cardiac Arrest Care
- Cerbrovascular Accident (Stroke)
- Transient Ischemic Attack (TIA)
- CVA Assessment Scales
- Pathophysiology of Shock
- Types of Shock
- Stages of Shock
- Care for Shock
9. Hemorrhage and Soft Tissue Trauma
- Infection
- Dressings and Bandages
- Stitches and Sutures
- Tourniquets
- External Bleeding
- Internal Bleeding
- Open Wounds
- Closed Wounds
- Burns
- Major Soft Tissue Trauma
- Types of Musculoskeletal Injuries
- Splints
- Slings
- Signs and Symptoms of Musculoskeletal Injuries
- Upper Extremity Injuries
- Lower Extremity Injuries
11. Chest, Abdominal and Pelvic Injuries
- Chest Injuries
- Rib Fractures
- Hemothorax
- Pneumothorax
- Subcutaneous Emphysema (SCE)
- Penetrating Chest Injuries
- Abdominal Injuries
- Evisceration
- Abdominal Aortic Aneurysm (AAA)
- Pelvic Injuries
- Pelvic Binding
- Genital Injuries
- Mechanism of Injury for Head and Spinal Injuries
- Head Injuries
- Skull Fractures
- Objects Impaled in the Skull
- Injuries to the Brain
- Cerebral Hematoma
- Spinal Injuries
- Spinal Motion Restriction (SMR)
- Care for Serious Head and Spinal Injuries
- Rapid Extrication
- Removing Helmets and Other Equipment
13. Acute and Chronic Illnesses
- Altered Mental Status
- Syncope
- Diabetic Emergencies
- Seizures
- Types of Seizures
- Epilepsy
- Peritonitis
- Appendicitis
- Bowel Obstruction
- Gastroenteritis
- Kidney Stones
- Peptic Ulcers
- Gastrointestinal Bleeding (GI)
- Urinary Tract Infection (UTI)
- Poison Control Centres
- Recognizing Poisoning
- General Care for Poisoning Emergencies
- Ingested Poisons
- Inhaled Poisons
- Absorbed Poisons
- Injected Poisons
- Substance Misuse and Abuse
- Crowd Management Agents
- Temperature Homeostasis
- Heat-Related Illness
- Heat Cramps
- Heat Exhaustion
- Heat Stroke
- Cold-Related Illness
- Hypothermia
- Frost Nip
- Frostbite
- Drowning
- Cold-Water Immersion and Drowning
- High-Altitude Illness
- SCUBA-Related Illness
- Physiology
- Barotrauma of Descent
- Barotrauma of Ascent
16. Pregnancy, Labour, and Delivery
- Pregnancy
- The Birth Process
- Assessing Labour
- The Labour Process
- Preparing for Delivery
- Assisting with Delivery
- Caring for the Neonate and Mother
- Care and Assessment for the Neonate
- Caring for the Mother
- Midwives and Home Births
- Complications during Pregnancy
- Spontaneous Abortion
- Premature Labour
- Ectopic Pregnancy
- Third Trimester Bleeding
- Complications During Childbirth
- Prolapsed Cord
- Breech Birth
- Limb Presentation
- Multiple Births
- Pediatric Patients
- Stages of Development
- Anatomical and Physiological Differences
- Assessing the Pediatric Patient
- Other Pediatric Conditions
- Geriatric Patients
- Dementia and Alzheimer's Disease
- Osteoporosis
- Bariatric Patients
- Palliative Patients
- Patients with Disabilities
- Psychological Crisis
- Suicide
- Assault
- Death and Dying
- Mental Health Crises
- Anxiety
- Depression
- Psychosis
19. Reaching, Lifting, and Extricating Patients
- Gaining Entry to Buildings
- Motor Vehicles
- Stabilizing Vehicles
- Accessing the Patient
- Moving Patients
- Body Mechanics
- Stretchers and Lifting Devices
- Lifting and Moving a Stretcher
- Bariatric Patients
- Emergency Vehicle Maintenance and Safety Check
- Removing a Vehicle from Service
- Beginning and Ending a Shift
- Safe Vehicle Operation
- Air Medical Transportation
- Patient Considerations
- Landing Site Preparation
- Ground Safety Precautions
- Medical Evacuation from a Ship
- Preparing the Patient for Transfer
21. Multiple Casualty Incidents
- Organizing Resources
- Caring for the Ill or Injured
- Triage
- CBRNE Emergencies
- Types of Agents
- Methods of Dissemination
- Scene Assessment
- Establishing Perimeters
- Triage in a CBRNE Incident
- Control of Contaminated Casualties
- Transporting CBRNE Patients
- Psychological Impact of CBRNE Events
- Assisting with Medication vs Administering
- Six Rights of Medication
- Pharmacological Terminology
- Routes of Drug Administration
- Pharmacokinetics
- Pharmacodynamics
- Intravenous (IV) Therapy Maintenance
- Preparing a Drip Set and Solution
- Calculating IV Flow Rates
- Changing an IV Bag
- Complications
- Discontinuing an IV Bag
- How to Administer Medication Intranasally
- Guidelines for Injections
- Disinfection
- Maritime Occupational Health and Safety Regulations (MOHS)
- Sterilization Techniques
- Managing Dangers at the Scene
- Toxicological Hazards on Board a Ship
- Psychological Well-Being of Seafarers
- Medical Care of Rescued Persons
- Radio Medical Advice
- Transfer and Transport
- Marine Pharmacology
- Medications and Health Supplies Carried on Board
- Drugs Requiring Medical Advice
- Roles and Responsibilities of the Advanced First Aid Attendant
- Responsibilities of the Employer and Other Employees
- Return-to-Work Protocol
- Workplace First Aid Equipment
- Workplace First Aid Transportation
- Regulations and Documentation
- Workplace Occupational Health and Safety Regulations
- Workplace Hazardous Materials Information System
- Documentation
- Typical Workplace Injuries
- Workplace Injuries
- Appendix A: Abbreviations for Documentation
- Appendix B: Sample Ambulance Equipment List
- Appendix C: The Phonetic Alphabet
- Appendix D: Medical Terminology
Basic Life Support Field Guide
.jpg)
Canadian Red Cross Basic Life Support Field Guide. Utlized by BLS, FR, EMR, Oxygen Therapy and Airway Management course students in Kelowna and Vancouver, BC.
The Canadian Red Cross Basic Life Support Field Guide reference manual is a pocket-sized, spiral bound 52 page, full-color text book with a soft red and white cover. The exterior cover and interior pages of the BLS Field Guide are made of a water resistant paper material, so you can keep it with you in the rain or wet environments without worry. The Basic Life Support Field Guide is available in PDF format as a downloadable resource for your mobile device, and in printed edition for Basic Life Support, First Responder, Emergency Medical Responder and Advanced First Aid course students.
The BLS Field Guide can also be purchased or downloaded by anyone with an interest in the most current and scientifically valid high-performance team based CPR-AED practices in Canada.
BLS Field Guide Contents:
Part 1. Introduction to Basic Life Support
- Basic Life Support Terminology
- Legal Issues
- Consent
- Implied Consent
- Responsive Patients
- Unresponsive Patients
- Children
- Abandonment
- Advance Directives
Part 2. Basic Life Support Skills
- Glove Removal
- Primary Assessment
- CPR
- Airway Obstruction
- Assisted Ventilation
- Anatomical Terminology
- Opening the Mouth
- Airway Adjuncts
- Suction
- Pulse Oximetry
- Pulse Oximeter Ranges and Values
- Supplemental Oxygen
- Oxygen Cylinders
- Oxygen Regulators
- Duration of Flow
- Oxygen Delivery Devices
- Administering Oxygen
- Special Considerations
- Trauma
- Hypothermia
- Opioid Overdose
- Anaphylaxis
- Six Rights of Medication
- High-Performance CPR
- Post-Cardiac Arrest Care
- High-Performance Team Communication
- Post-Event Debrief
BC EMALB Examination Guidelines
.jpg)
Summary of BC EMALB Examination Guidelines for Emergency Medical Responder course participants in Kelowna and Vancouver, BC.
The Canadian Red Cross, BC Ambulance Service and BC Emergency Medical Assistant's Licensing Board follow the National Occupational Competency Profile (NOCP) for most EMR skills, as endorsed by the Paramedic Association of Canada (PAC). EMALB, the agency responsible for Licensing evaluations in British Columbia, has additional, sometimes contradictory requirements to successfully complete their practical scenario examinations. These requirements are outlined in the EMALB British Columbia Provincial Examination Guidelines booklet. Whenever the BC EMALB Examination Guidelines contradict or supplement the information provided in the Canadian Red Cross Emergency Care for Professional Responders text book, the EMALB Examination Guidelines take precedence and overrule any other interpretations.
The Emergency Medical Assistants Licensing Board British Columbia Provincial Examination Guidelines for Primary Care Paramedics and Emergency Medical Responders is produced and updated by the BC EMALB team of medical professionals and advisors. The purpose of the Guidelines document is provide insight and consistency for Emergency Medical Responder and Primary Care Paramedic course students preparing for their EMALB practical scenario evaluations.
The BC EMALB Examination Guidelines are updated frequently, so it's a good practice to revisit and review the Guidelines often, particularly as you get close to your scheduled EMALB EMR Licensing examinations.
.jpg)
Cheat Sheet for Canadian Red Cross Emergency Medical Responder courses, with BC EMALB Licensing eligibility in Kelowna and Vancouver, BC. Medi-Pro First Aid's Emergency Medical Responder (EMR) Cheat Sheet will provide you with quick and easy access to some of the most critical and frequently referred to information throughout your Kelowna EMR Course.
The visually compelling Charts and Summaries can simplify the more complex principles and procedures you'll need to be familiar with as an Emergency Medical Responder operating in British Columbia.
While most of the EMR Cheat Sheet is based on information extrapolated from the Canadian Red Cross Emergency Care for Professional Responders EMR text book, some of the information is based on the BC specific policies and guidelines stipulated by the British Columbia Emergency Medical Assistant's Licensing Board (BC EMALB) and BC Emergency Health Services (BCEHS). The EMR Cheat Sheet can be an invaluable resource for you to keep track of the specific local protocols that will help ensure sucess in your EMR course and throughout your corresponding EMALB Licensing examinations.
EMR Cheat Sheet contents include...
- EMR Patient Assessment Model
- CPR Compression to Ventilation Ratios
- High Performance "Pit Crew" CPR
- CPR in Transport (Treatable CPR)
- Oxygen Cylinder Calculations
- Oxygen Flow Rates
- Glasgow Coma Scale
- APGAR Assessment for Newborn Infants
- Adminitration of Medications vs Assisting with Medications
- The 6-Rights of Medication
- Urgent Transport Critical Interventions that require History and/or Vital Signs
- Common Units of Measurement
- Assisted Ventilations
- Weight Estimation for Pediatric Patients
- ATMIST AMBO Patient Care Hand-Off
- BCEHS Treatment Guidelines Compared to National Occupational Competency Profiles
- Critical Findings
- Epinephrine Administration by Auto-Injector
- Acetaminophen Administration
- Ipbuprofen Administration
- Glucagon Administration by Intra-Muscular Injection
- Glucagon Administration by Intra-Nasal Spray
- Glucogel Administration (Parenteral)
- T-Pod Pelvic Binder Application
- Kendrick Extrication Device (KED) Strapping Sequence
- Entonox Indications/Contraindications Mnemonics
- Entonox Administration Procedures
- Sager Traction Splint Procedures
- Glucogel Administration Guidelines
- Head-to-Toe Assessment Mnemonics
- Average Vital Signs
- Hypotension (Low Blood Pressure)
- Relevant SAMPLE and Mechanism of Injury Data
- Intravenous Drip Set Calculations
- Common IV Solutions
- Common IV Complications
- Common Medical Terms
- F-A-S-T V-A-N Stroke Assessment Mnemonics
- NEXUS Spinal Motion Restriction Decision Matrix
- Naloxone (Narcan) Administration Protocols
.jpg)
You will access and complete the BC EMALB Scope of Practice modules through the Canadian Red Cross online learning platform. As you near the completion of your Emergency Medical Responder course, you will recieve a course activation email from the Canadian Red Cross MyRC elearning platform. From there, you can access and complete your online Scope of Practice course modules through your Canadian Red Cross MyRC Profile.
Once you have completed the profile creation process, accessed your Canadian Red Cross MyRC profile, and successfully activated the British Columbia Emergency Medical Responder Scope of Practice Update modules in the "My Online Courses" section, you will be able to move through the individual modules at your own pace. You can start and stop as often as you like, and you can pick up where you left off later.
You can review and re-complete any of the chapters as many times as you like, regardless of whether or not you were successful on the first try. The course will remain accessible to you, through your MyRC profile, at any time. You can review any of the information and learning outcomes whenever you want to brush up on your Standard First Aid knowledge and understanding.
Once you have successfully completed all the modules you can access, download and print your certificate of completion for the online portion (note that this is different from the actual Emergency Medical Responder certificate you will receive after completing the in-person classroom sessions). Although you can always download the certificate again later, through your MyRC profile, Medi-Pro recommends that you store a pdf copy of your certificate on your hard-drive/cloud storage server for quick reference and proof of completion.
Step-by-Step Instructions...
- Sign in to your MyRC profile at myrc.redcross.ca
(Click here for instructions on setting up your MyRC Profile for the first time, if you haven't done so already) - Click the "My Profile" tab, then select "My Online Courses"
- Click "Activate" next to the British Columbia Emergency Medical Responder Scope of Practice Update module
- Verify your preferred language
- Click "Enter Course"
Contact the Canadian Red Cross Contact Center for assistance, if you have technical difficulties accessing your MyRC Profile or the EMALB EMR Scope of Practice modules.
- email: myrcsupport@redcross.ca
- tel: 1-877-356-3226
Scope of Practice Modules
- Introduction
- Section 1: Anatomy of an EMS Call
- Section 2: First Responder Schedule One (Core Licence Services) Gap Module
- Section 3: First Responder Schedule Two - Vital Signs Endorsement Module
- Section 4: First Responder Schedule Two - Medications Endorsement Module
- Section 5: Emergency Medical Responder Schedule Two - Medications Endorsement Module
- Conclusion
Introduction
- Navigation
- Introduction: Module Overview
- Background
- Development Process
- Educational Approach
- Evaluation Strategy and Course Completion Requirements
- References
- Summary
Section One: Anatomy of an EMS Call
- Anatomy of an EMS Call: Module Overview
- Scene Survey/Rescue Scene Evaluation
- Primary Survey
- Transport Decision
- Secondary Survey
- Ongoing Survey/Protocols/Treatments/Reporting
- Summary
Module Two: First Responder Schedule One (Core Licence Services) Gap Module
- First Responder Schedule One (Core Licence Services): Module Overview
- Introduction
- Nasopharyngeal Airways (NPA)
- Serious Hemorrhage Management/Wound Packing
- Fracture Management/Pelvic Binding
- Lifting/Loading and Extrication/Evacuation
- Knowledge Evaluation
- Summary
Module Three: First Responder Schedule Two - Vital Signs Endorsement Module
- First Responder Schedule Two - Vital Signs Endorsement: Module Overview
- Introduction
- Pulse Oximetry
- Blood Pressure Assessment
- Glucometry
- Knowledge Evaluation
- Summary
Section Four: First Responder Schedule Two - Medications Endorsement Module
- First Responder Schedule Two - Medications Endorsement: Module Overview
- Introduction
- Assisting Patients Their Own Prescribed Medications
- Administering Epinephrine Via Auto-Injector to a Patient in Anaphylaxis
- Administering Opioid Antagonists to a Patient in Opioid Poisoning
- Administering an Anti-Hypoglycemic Agent to a Hypoglycemic Patient
- ASA/Oral Analgesia/Topical Pro-Coagulant Agents
- Knowledge Evaluation
- Summary
Section Five: Emergency Medical Responder Schedule Two - Medications Endorsement Module
- Emergency Medical Responder Schedule Two - Medications Endorsement: Module Overview
- Introduction
- Intramuscular Administration of Epinephrine
- Administration of Brochodilators by Inhalation and Nebulization
- Knowledge Evaluation
- Summary
Section Six: Conclusion
- Next Steps
- Quick Recap
- Reflection
.jpg)
Downloads and online, web-based resources for Emergency Medical Responder courses and BC EMALB Licensing eligibility in Kelowna and Vancouver, BC. Emergency Medical Responder certification training, EMALB Licensing preparation, and the provision of emergency medical care as a professional responder all involve far more that simply learning something once in the classroom. The paramedic profession is extremely dynamic and requires a lifetime committment to remaining up to date on the most current EMR protocols, guidelines, science, and practices.
This means that you will need to learn how to find the documented information and guidelines related to your Emergency Medical Responder training and verify that what you remember learning is still considered a current practice. In addition to the documents and textbooks already outlined above, you will need to access and refer to several other online resources as you prepare to be successful throughout your Emergency Medical Responder training and BC EMALB Licensing Evaluations.
Many of these resources can be downloaded and printed or saved, and some are only available online, through a desktop computer, laptop, or mobile web browser. Although you may find it convenient to download many of these documents and print them for easy reference, you should make a habit of frequently revisiting the source material online to make sure you are utilizing the most current materials.
EMR Certification Requirements
.png)
Medi-Pro First Aid's Emergency Medical Responder courses are facilitated in a friendly, learner-centered environment, with the skills and principles presented in a simple and straight forward manner. Your Emergency Medical Responder course Instructor will do everything possible to ensure that you meet national Canadian Red Cross, and provincial BC EMALB benchmarks for Emergency Medical Responder certification and provincial Licensure.
Key Emergency Medical Responder and Basic Life Support topics are presented in a distilled and relevant context, which makes them easy to understand and remember. A mix of interactive group activities and self-application make the paramedical principles easy to understand and fun to learn. Most of the course is dedicated to physical skills and hands-on learning which involve clear demonstrations immediately followed by opportunities to apply, practice, repeat and reinforce the Emergency Medical Responder skills with realistic equipment.
In order to receive Canadian Red Cross Emergency Medical Responder certification, which is valid for 3 years from date of completion, you must meet the following course attendance, performance and participation requirements.
- Attendance in 100% of the course (this includes arriving, and returning from all breaks, on time)
- Earnest and mindful participation in all activities, skills, and scenarios
- Respectful behaviour towards the Instructor all other participants Adherence to all classroom/facility health and safety guidelines
- Legible, accurate submission of your First & Last name and your preferred email address (this is required for Medi-Pro to process your EMR Certification through the Canadian Red Cross)
- Minimum 75% on a multiple choice Written Exam
- If required and appropriate, a second attempt at the Written Exam may be permitted on a case-by-case basis
- Successful completion of one Medical-based practical scenario Evaluation
- Successful completion of one Trauma-based practical scenario Evaluation
- If required and appropriate, a second attempt at the Practical Exams may be permitted on a case-by-case basis
Personal items to bring to your EMR course
.jpg)
Bringing a few essential items with you to class can make the entire Emergency Medical Responder course more enjoyable. This added level of comfort can also help ensure you learn and retain the EMR and BLS skills, as well as meeting all the certification requirements as you participate.
Making sure you can see and hear your instructor, classmates and multi-media presentations is important. Although our Instructors will speak clearly and our video/projector screens are large enough to ensure full classroom visibility, you must bring any corrective eyewear or hearing aides (with fresh batteries) that you might need with you in your first aid course. In some cases you might need reading glasses for your EMR text book and reading-based activities, or you may need corrective lenses to clearly view the videos, slideshows and instructor-led Emergency Medical Responder skill demonstrations.
If you normally require daily medications, you should definitely bring them with you to class, and adhere to your normal schedule. You might also find that your active participation in the first aid skills and activities throughout the day can increase your metabolic demands and the corresponding medication amounts. Basically, bring extra medications in case your needs increase throughout the day. It's better to have these with you and not end up needing them, rather than leaving them at home and wishing you had brought them. A few other suggestions include...
- All relevant books and printed resources
- Clean indoor footwear
- Reusable mug
- Refillable water bottle
- Food for meals and snacks through the duration of the course
- Clothing which allows for modesty, professionalism and comfort during physical activity
- Spare shirt and sweater in case of temperature changes or excessive sweating
- Medications that you might need throughout the day
- Glasses or contact lenses if required for reading
- Pen and notepad
- Kneepads if prolonged and repeated physical activities in a kneeling position may cause you discomfort.
- Lightly scented deodorant
.jpg)
Your Emergency Medical Responder course will be conducted in an "Adult Learning" format, which means that you will be free to excuse yourself from the classroom at any time, if you need to use the washroom, answer an urgent phone call/text, or attend to any other emergent matter that can't wait until the next scheduled break.
Medi-Pro administration and Instructors recognize that unanticipated circumstances may occur outside the classroom which require your immediate attention, but will ask that you limit these distractions to only those that are essential, and to minimize the disruption to other participants.
If you become thirsty or hungry, you are encouraged to keep yourself nourished and hydrated in the classroom, provided this does not interrupt hands-on activities or interfere with others' safety, participation and learning. There will also be formal breaks scheduled throughout the day, which can be utilized for communications, snacks, lunch and beverages.
- There will be a 15 minute break approximately every 2 hours, depending on classroom progress and participant pacing.
- You will need to arrive with enough food and drinks to remain hydrated and nourished for the duration of each session
- There will be one 30-minute Lunch break every day at or around noon.
- Access to local stores and restaurants may be limited.
- Use of electronics is discouraged except during breaks or when the Instructor specifically deems it appropriate
- Smoking is prohibited except for designated times and areas
- The use of vaporization products and devices is prohibited except for designated times and areas
- Consumption of alcohol in the classroom and grounds is prohibited
- Consumption of cannabis in the classroom and grounds is prohibited, except where medically required
- Impairment, as observed or presumed by the Instructor, will preclude you from participation and certification, regardless of the legality of any substances involved
.jpg)
Participating in your Canadian Red Cross Emergency Medical Responder course in Kelowna or Vancouver, BC will involve working in close proximity with your classmates. Respectful physical contact is an unavoidable component of hands-on First Aid training. Out of consideration for your classmates, please arrive with hygeine, professionalism, and the comfort of others in mind.
Although it is impossible to define the term "appropriate" when it comes to clothing choices, there are few universal considerations. Slogans, logos, or images that could reasonably be categorized as objectively offensive or controversial must not be worn or displayed. Clothing which is soiled to the point that incidental contact may contaminate other clothing, equipment or furnishings are not acceptable in the classroom. Cothing or hygeine products which emit a strong odor may make it difficult for other participants to concentrate or enjoy the lessons and activities.
The health of all participants and staff is of paramount importance, so if you are feeling sick, or suspect that you may be contagious of any viral or bacterial infection, you must not attend the classroom. In cases of last minute cancellations related to unpredicted illness, Medi-Pro will make reasonable efforts to reschedule your course for a later date, when you are no longer sick/contagious.
- Hygeine and beauty products should be unscented or lightly-scented only
- Jewellery or accessories that could cause injury or entanglement may need to be removed (please do not bring expensive jewellery or irreplaceable heirlooms)
- Longer hair needs to be secured in a way that prevents it from getting into others mouths and eyes
- Your clothing should allow you to participate with comfort and consideration for others
- Slogans or images that might be considered controversial, disrespectful or confrontational should be avoided
- Some types of clothing may restrict your ability to participate or compromise your classmates' comfort.
- Although it is impossible to define every aspect of the term "inappropriate" ahead of time, we ask that you take this into consideration when making your choices
.jpg)
Participating in your Canadian Red Cross Emergency Medical Responder course in Kelowna and Vancouver, BC will involve significant physical activity. If you have medical conditions, physical injuries or limitations that might compromise your ability to safely participate in these physical activities, you must notify your Instructor at the start of your course. Your Canadian Red Cross certified Instructor will make reasonable efforts to adapt and accomodate your limitations, but it is your responsibility to decide whether or not you can safely complete any particular task.
Your Canadian Red Cross Emergency Medical Responder course Instructor will balance the classroom between interactive theory components and hands-on physical activities, and you must actively participate in all the sections to successfully complete your EMR course. The physical requirements are not objectively intensive or difficult, but they do involve specific and repetitive movements. If you have any significant restrictions on your movement or exertion capacity, you should contact Medi-Pro well in advance of your scheduled course date to ensure that we can accommodate your limitations and provide the greatest opportunities for successful participation. Physical activities typical of Canadian Red Cross Emergency Medical Responder courses include...
- Kneeling on the ground
- Laying face-down on the ground
- Laying face-up on the ground
- Walking up and down stairs
- Rolling and lifting an adult sized classmate
- Performing CPR chest compressions on a CPR mannequin
- Using a pocket mask with a one-way valve to inflate the lungs of a CPR mannequin
- Sitting for 15-30 minutes at at time
- Standing for 15-30 minutes at a time
- Tying simple knots
- Tearing medical tape
Code of Conduct in EMR courses
EMR Course Skills & Principles
Get the most out of your Kelowna Emergency Medical Responder course by familiarizing yourself with the EMR course content, schedule, skills and structure. The content, principles, skills and information covered in your Kelowna Emergency Medical Responder training is broken into specific sections in your EMR printed materials and online resources. The extensive EMR level information provided in your Canadian Red Cross Emergency Care for Professional Responders reference manual is divided numerically into Sections 1 to 24, with Appendices alphabetically labelled. You are also provided with many other supplements, downloads and online resources which help put all this information into context, and provides guideance on how these skills and principles are specifically applied in British Columbia, as required by BCEHS and EMALB Licensing. These resources are referenced in Sections A, B, C, and D in your EMR Study Guide.
The classroom topics and content covered in each day of your Kelowna EMR course will generally correspond with specific sections of your Emergency Care Manual and supplemental resources. The sequence of topics covered in the EMR classroom will not necessarily follow the sequence in which they are presented throughout the Emergency Care for Professional Responders text. The daily schedule for every EMR course is subject to change and revision based on the needs of that particular EMR class.
- EMR concepts, principles, and skills are introduced in a simplified context and logical sequence.
- The EMR course starts with basic drills, and builds towards more complex scenarios with an emphasis on clinical decision making as participant skill levels and confidence improve.
- Stand-alone skill components are introduced and reinforced, then integrated into realistic situations and circumstances.
- Intensity, workload and student responsibilities increase as the EMR course progresses, with developing emphasis on clinical decision making abilities and adaptive skill application.
.jpg)
The Patient Assessment Model is the foundation of your Emergency Medical Responder training. The ability to intuitively follow a consistent and logical, yet flexible and adaptive process to assess your surroundings and the patient is the single most important key to being successful in your EMR course, your subsequent BC EMALB Licensing Evaluations, and most importantly in delivering high quality patient care as a professional medical responder.
A significant part of learning and practicing the EMR Patient Assessment Model also involves becoming familiar with the professional medical responder equipment available to you, and becoming increasingly proficient in their use. Some pieces of equipment, such as oxygen masks, blood pressure cuffs, stethoscopes and pulse oximeters are utilized during almost every patient interaction. Other types of equipment are bit more specialized, such as oropharyngeal airways (OPAs), nasopharyngeal airways (NPAs), blood glucose meters, and airway suction devices, and only utilized when necessary for patient assessment and care.
Although you will be provided with enough theory and background information to make use of these tools and processes, as much time as possible of your EMR course is dedicated to hands-on practice and reinforcement of these fundamental skills. Each time you practice applying these skills in a relevant and practical manner, the more proficient you will become and the more muscle memory you will develop for the future. Patient Assessment Model componenents, skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- EMR Assessment Model
- Scene Assessment
- EMR Equipment
- Paramedic Jump Kits
- EMR Scene Assessment
- EMR Primary Assessment
- EMR Secondary Assessment
- EMR Ongoing Assessment
- Patient Transport
- Medical Oversight
- Direct Medical Control
- Offline Medical Control
.jpg)
Assessing the scene that you are about to enter is the most important step in ensuring your own personal safety, as well as asserting and maintaining control over the situation to improve operational efficiency and provide quality patient care.
In some cases, such as an ongoing fire, hazardous materials spill, or confined space you may need to make a difficult but crucial decision to move or remain outside the hazardous area until more specialized rescue teams can mitigate the problem and/or bring the patient to you in a safe area. In other cases, such as a motor vehicle collision, you may be able to safely access the patient but require assistance from other agencies to extricate and transport the patient.
In all cases and at all times, you must maintain acute operational awareness of your surroundings and the changing conditions in which you are working. Taking a few extra seconds to meaningfully and thorougly evaluate the situation, and engaging all the required resources and personal protective equipment will save time overall and most importantly help ensure positive outcomes and the safety of everyone on the scene.
Scene Assessment, skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to perform a Scene Assessment
- How to assess the scene for hazards
- How to assess the environment of your surroundings
- How to assess the mechanism of injury
- How to assess the number of patients
- How to assess the need for additional resources on scene
- How diseases are transmitted
- Occupational Vaccinations and Booster Shots
- How to don and doff your Personal Protective Equipment (PPE)
- How to don and doff medical examination gloves
- How to don and doff protective eye-wear
- How to don and doff a face shield
- How to don and doff a medical examination gown
- How to call for Fire Rescue
- How to call for Haz-Mat Response
- How to call for Advanced Life Support
- How to call for Air Ambulance
- How to call for High Angle Technical Rescue
- How to call for Confined Space Rescue
- How to perform a seat-carry
- How to perform a clothing/blanket drag
- How to perform a walking assist
- The principle of Life-Over-Limb
.jpg)
The Primary Assessment survey is your first opportunity to check the patient for any obvious and immediately life-threatening injuries or conditions, and perform timely interventions to mitigate those injuries in a manner that stops or slows down any progressive decline in the patients condition. Airway, Breathing, and Circulation emergencies are generally the most crucial to identify and deal with in the first few minutes of your assessment. If there are any urgent problems with the upper airways, respiratory distress, or deadly external/internal bleeding, the Primary Assessment process gives you a systematic and efficient method to find and address those problems within a minute or two of arrival at the patient's side.
At the end of your Primary Assessment, you will pause to reflect on everything that you've already identified, review any outstanding or potentially life-threatening issues and initiate critical interventions such as OPA/NPA insertion, oxygen therapy, bleeding control, shock management and administration of medications as appropriate. You will also make your initial transport decision and determine whether immediate transport to definitive clinical care is a higher priority than continued and more thorough on-scene assessment. Although you will continuously receive, collect and consider new information as it changes or becomes available, the decisions you make in the first few minutes based on your Primary Assessment findings will set the tone for your overall patient care and transport priorities. Primary Patient Assessment, skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to conduct an EMR Primary Assessment
- How to measure and insert an Oropharyngeal Airway (OPA)
- How to measure and insert a Nasopharyngeal Airway (NPA)
- How to assemble an Oxygen cylinder and regulator
- How to use a Simple Oxygen Mask
- How to use a Non-Rebreather Oxygen Mask
- How to use a Nasal Canula
- How to place patients in the Recovery Position
- How to find and assess the Radial pulse
- How to find and assess the Carotid pulse
- How to check Skin condition
- How to perform an EMR Rapid Body Survey (RBS)
- Rapid Transport Category (RTC) criteria
- How to conduct the EMR Secondary Assessment with an Unresponsive Patient
- How to conduct the EMR Secondary Assessment with a Responsive Patient
.png)
The Secondary Assessment survey is conducted on scene when there are no urgent, life-threatening conditions which make rapid transport a higher priority. In cases of urgent transport, the Secondary Assessment is conducted enroute to the hospital, in the back of the ambulance. In some cases, where transport options are delayed or not available, you might conduct the Secondary Assessment on scene with life-threatening conditions, but transport to definitive clinical medical care is always more crucial when life-threatening injuries are present.
Components of a thorough, methodical and comprehensive Secondary Survey include an Interview of the patient and/or bystanders, family members, or witnesses, measurement of a complete set of Vital Signs, and a Head-to-Toe physical examination. Individually, each piece of data collected during the Secondary Assessment may not be significant or revelatory, however the information will collectively help form a clearer picture of all the potentially life-threatening, limb-threatening, or debilitating factors present and whether the patient's overall condition is improving or declining. Secondary Patient Assessment, skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to conduct an EMR Secondary Assessment
- How to measure and interpret SpO2 using a Pulse Oximeter
- How to perform a Capillary Refill circulation check
- How to conduct a patient interview following the S-A-M-P-L-E and O-P-Q-R-S-T mnemonic
- How to assess patient Signs and Symptoms
- How to assess patient Allergies
- How to assess patient Medications
- How to assess patient Previous relevant medical history
- How to assess patient's Last intake of food or fluids
- How to assess the Events leading up to current circumstances
- How to assess the Onset of pain or discomfort
- How to assess Provocation and Palliation of pain or discomfort
- How to assess the Qualities of pain or discomfort
- How to assess the Radiation of pain or discomfort from one anatomical area to another
- How to assess Severity of pain or discomfort on a subjective scale of 1-10
- How to assess the Timing of pain or discomfort
- How to assess Level of Responsiveness using the Glasgow Coma Scale (GCS)
- How to use a Stethoscope
- How to use a Sphagmomanometer (Blood Pressure Cuff)
- How to assess Blood Pressure using the Palpation method
- How to assess Blood Pressure using the Auscultation method
- How to assess Respiration rate, rhythm and character
- How to assess Radial Pulse rate, rhythm and character
- How to assess blood glucose levels (CapBgL) using a Glucometer
- How and when to assess a patient's Vital Signs
- How to assess patient Pulse rate, rhythm, and character
- How to assess patient Respiratory rate, rhythm, and character
- How to assess patient Pupils for equal size and reaction to light
- How to assess patient Body Core Temperature
- How to Auscultate the chest to check for adventitious breathing sounds
- How to assess the Pedal pulse and Distal Extremity Circulation
- How to conduct an EMR Head-to-Toe Physical Examination
- How to conduct an EMR Head-to-Toe System Check
.jpg)
After you have conducted a thorough Secondary Assessment and treated any injuries or conditions identified, you will move into the Ongoing Assessment phase of your patient care. You will continuously reassess your surroundings and the patient's condition until the patient has been transferred to another (usually higher) level of care. This includes re-measuring the Vital Signs every 5 minutes if there are life-threatening conditions, or every 15 minutes if the injuries are minor in nature. You will also ask many of the S-A-M-P-L-E and O-P-Q-R-S-T Interview questions to see if the patient remembers anything new or is experiencing a change to their levels of discomfort. Continued, periodic reassessment will help you determine if there are any patterns in the changes to the patient's condition, such as gradually decreasing blood pressure or increasing oxygenation levels which can show overall improvement or decline and/or indicate specific underlying conditions.
The Ongoing Assessment phase also includes complete and accurate documentation of all your findings on a Patient Care Report. The report may be hand written on paper, or an electronic record stored and uploaded through a mobile device. Either way, an accurate and timely Patient Care Record forms a significant component of your overall patient care and contains information that may be potentially vital to the next level of care in forming an effective diagnosis and treatment plan. You will provide a brief but relevant verbal summary of your findings, actions and opinions regarding your patient when you hand them over to a higher level of medical treatment or another agency. Ongoing Assessment, skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to conduct an EMR Ongoing Assessment
- Patient Care Records and Reports
- Legal implications of Patient Care Records
- How to fill out a Patient Care Report
- How to ensure the Patient Care Report information is passed along
- Transferring patient care to another level of care or agency
- How to verbally transfer patient care using the A-T-M-I-S-T A-M-B-O summary mnemonic
- How to summarize the patient's Age, Name, and Date of Birth
- How to summarize the Time and Onset of the patient's Signs/Symptoms/Injuries
- How to summarize the patient's Mechanism of Injury/Medical Complaint
- How to summarize the patient's Ijuries and your physical examination findings
- How to summarize the patient's Vital Signs
- How to summarize the patient's Allergies
- How to summarize the patient's Medications
- How to summarize the patient's Background
- How to summarize any Other information relevant to ongoing care of the patient
.jpg)
Respiratory Illnesses such as asthma, COPD, pneumonia, emphysema, and congestive heart failure are very common medical emergencies that you may encounter as a paramedic/professional responder. Other medical conditions such as anaphylaxis and anxiety, and opioid overdose can also cause breathing problems and create respiratory distress. In your EMR course you will learn and practice a universal approach to providing patient care for someone experiencing Respiratory Distress, as well many techniques to mitigate specific respiratory problems as they are individually assessed.
The use of a pulse oximeter, supplemental oxygen therapy equipment, and particularly the efficient and effective use of a Bag-Valve-Mask (BVM) to assist ventilations and deliver high-flow oxygen are particularly relevant for a patient experiencing respiratory distress or respiratory arrest. In addition to these measures, you may commonly need to assist a patient with their medication such as ventolin, salbutamol, epinephrine, and/or benadryl. In the event that your patient is breathing too fast, too shallow, or too slowly to be effective, you will need to breath for them with a Bag-Valve-Mask, which is most efficient with two trained professional rescuers. Respiratory Distress and Respiratory Arrest skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to use a Bag-Valve-Mask (BVM) with one responder
- How to use a Bag-Valve-Mask with two responders
- How and when to Assist Ventilations
- How to provide care for a patient in respiratory arrest
- The 6 Rights of Medication
- How to recognize the signs and symptoms of Asthma
- How to provide care for a patient with Asthma
- How to administer Salbutamol (Ventolin) with a nebulizing mask
- How to administer Salbutamol (Ventolin) with a metered dose inahaler (MDI) and spacer
- How to recognize the signs and symptoms of Chronic Obstructive Pulmonary Disease (COPD)
- How to provide care for a patient in Respiratory Distress
- How to recognize the signs and symptoms of Anaphylactic Shock (Anaphylaxis)
- How to provide care for a patient experiencing Anaphylaxis
- How to administer epinephrine using a metered dose inhaler (Epi-Pen)
- How to administer epinephrine by weight-based intramuscular injection (IM)
.jpg)
Cardiac arrest is another very common medical emergency, which requires the performance of Cardiopulmonary Resuscitation (CPR) and the use of an Automated External Defibrillator (AED) in an attempt to revive a patient without a pulse. Your EMR training course includes learning and practicing CPR at the Basic Life Support (BLS) level. BLS includes a team based "pit-crew" approach to CPR, the use of supplemental oxgyen, an AED, and high-performance roles performed and coordinated efficiently by each member of your medical response team.
High fidelity CPR begins with quick recognition of cardiac arrest followed by immediate chest compressions at a depth of at least 2 inches (for an adult) and at a rate of 100 - 120 compressions per minute. Compressions should be followed by the application and use of an Automated External Defibrillator (AED) which can administer an electrical shock to the heart and "reset" it to normal function when Ventricular Tachycardia or Ventricular Fibrillation are analyzed and detected. The next priority for quality CPR is providing ventilations/rescue breaths using a Bag-Valve-Mask with high-flow oxygen set to 15 liters per minute (lpm). The national standard for CPR compression to ventillation ratios is 30 compressions for every 2 breaths (30:2), however some specific agencies in BC may follow a regional guideline which stipulates a 10:1 ratio instead.
For purposes of performing CPR, anyone over the age of 9 (and/or the onset of puberty) is considered an Adult. Patients between the ages of 1 year and 9 years are considered Children, and patients under the age of 1 are considered Infants. There is an additional sub-set of Infants who are less than 28 days old referred to as Neonates. Although the basic principles of high fidelity CPR remain the same across patients of all ages, there are some logistical differences in performing CPR on smaller bodies. These differences include modified compressions, smaller ventilations, and performing CPR at a compression:ventilation ratio of 15:2. Basic Life Support and Cardiac Arrest management skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to perform CPR & AED for an Adult patient
- How to perform CPR & AED for a Child patient
- How to perform CPR & AED for an Infant patient
- How to perform CPR & AED for a Neonatal patient
- How to perform high-performance Pit Crew style CPR and AED
- How to perform Basic Life Support (BLS)
- How to perform CPR on the move and in transport
- How to provide care for a Responsive Choking Adult
- How to provide care for a Responsive Choking Child
- How to provide care for a Responsive Choking Infant
- How to use a manual airway suction device
- How to perform CPR & AED with an ongoing airway obstruction
.jpg)
The spinal cord is a cable of nerves extending from the base of the brain-stem down to the rest of the body, travelling through the vertebrae of the spinal column and branching out in nerve fibres to every area of the body. Signals that allow movement and function move through spinal cord from the brain to the rest of body, and sensory signals are carried from the nerve ends back to the brain through the same nerves. If an injury causes the spinal cord to become severed, the signals are no longer sent or received in either direction and sensory and motor deficits can permanently occur.
A significant portion of your EMR training course involves learning and practicing the prinicples of Spinal Motion Restriction (SMR), the Canadian C-Spine Rules, and the National Emergency X-Radiological Utilization Study (NEXUS) protocols which replaced the older Spinal Immobilization approach. The new SMR guidelines and accompanying modified NEXUS protocols adopted by BC EMALB provide paramedics with more options and flexibility to provide patient care when spinal cord injury is suspected, but the complex decision matrix requires memorization and practice.
You will also get lots of hands-on practice with spinal grips, skills, and equipment such as the trapezius grip, head grip, modified trap squeeze, jaw thrust, c-spine collars, robertson orthopedic stretchers (clamshells), spine boards, spider straps, head rolls, and rescue pads. The ability to mix and match a large "library" of skills and equipment as best suited to the specific circumstances will allow you provide the best patient care possible for suspected spinal injuries in any emergency. Spinal Motion Restriction tools, skills and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- Anatomy and Physiology of Spinal Cord Injuries
- Anatomy and Physiology of Head Injuries and Concussion
- How to recognize the signs and symptoms of Head and Spinal Injuries
- How to provide Spinal Motion Restriction (SMR) for patients with suspected Head or Spinal Injuries
- How to apply the Canadian C-Spine Rules in BC
- How to apply the modified Nexus C-Spine Rules in BC
- How to perform a Jaw Thrust
- How to perform a Trapezius Squeeze
- How to perform a Head Grip
- How to perform a Modified Trapezius Squeeze
- How to perform a Sternal-Spinal Grip in a supine position
- How to perform a Sternal-Spinal Grip in a lateral position
- How to align the Head into a Spinal-Neutral position
- How to measure and apply a C-Spine Hard Collar
- How to roll a patient from a supine to lateral position while maintaining Spinal Motion Restriction
- How to roll a patient from a prone position to a supine position while maintaining Spinal Motion Restriction
- How to secure a patient to a Spineboard with Spinal Motion Restriction precautions
- How to secure a patient to a Robertson Orthopedic Stretcher (Clamshell Stretcher) with Spinal Motion Restriction precautions
- How to provide patient assessment and care with Spinal Motion Restriction precautions
.jpg)
Deadly bleeding is another significant type of injury that you will encounter as a paramedic, and you will learn and practice the most current effective techniques to control external capillary, venous and arterial bleeding. The simplest approach to controlling deadly bleeding is direct pressure with a dressing and a bandage. Dressing is any clean (preferrably sterile and absorbent) material that is placed directly against the wound and blocks the bleeding, while a Bandage is any material used to surround the dressing, keep it clean and dry, and bind it securely in place with sufficient pressure to staunch the blood flow. Triangular bandages, speed straps and abdominal pads are some of the most commonly utilized tools to achieve direct pressure.
In some cases, where direct pressure is ineffective or impractical a tourniquet may be utilized to controll bleeding through Indirect Pressure. A tourniquet is placed upstream of the wound or amputation and bound tightly enough around the humerus or femur to squeeze the brachial or femoral artery shut against the bone. A tourniquet is usually only necessary in the most extreme injuries such as amputations. Deadly Bleeding tools, skills and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- Capillary Bleeding
- Venous Bleeding
- Arterial Bleeding
- Amputational Bleeding
- How to control deadly bleeding with direct pressure using a bandage and dressing
- Clinical bandages and dressings
- Improvised bandages and dressings
- The value of keeping a wound clean
- When to replace bandages and dressings
- How to recognize when direct pressure is ineffective
- How to control deadly bleeding with indirect pressure using a commercial tactical tourniquet
- How to control deadly bleeding with indirect pressure using an improvised tourniquet
- Where to place a tourniquet
- When to remove a tourniqet
- How to use pro-coagulants
- How to perform wound packing
.jpg)
Fractures are injuries which cause any damage to bone structures, which can include cracking, chipping, splintering, complete breaks, and compound fractures where the broken bone ends protrude through the skin. Sprains are injuries to the ligaments which anchor the ends of two bones together, and usually involve stretching and/or tearing. Strains are injuries, which also usually involve stretching and/or tearing, to the tendons which hold muscles to bones. Dislocations are injuries that occur when two bone ends which normally connect are pulled out of alignment, usually involving a shoulder, knee, wrist, finger or toe.
When someone damages a bone or joint, the injury may be limited to just a fracture, sprain, strain or dislocation, but more often the injury is a combination of two or more of those conditions. For example, a fracture to an ankle bone will usually include some damage to the ligaments and tendons, and may even involve more than one bone. Regardless of the specific structures and tissues involved, an injury of this nature will usually present itself with universal signs and symptoms that include pain, tenderness, swelling and discoloration. It is not necessary to diagnose the specific types of inury/injuries to provide good first aid care.
Emergency medical care for fractures, sprains, strains and dislocations involves providing comfortable support for the injury, and preventing further aggravation or long-term complications. Injury stabilization and support is provided in the form of a splint, which can be created from many different materials and in many configuations. Ensuring that the patient remains as comfortable as possible, supporting the limb above and below the injury, and ensuring that circulation is not impaired are the main principles of splinting. It's important to note that although these types of injuries are not typically life-threatening, if the broken bones cut through the surrounding blood vessels, severe internal bleeding can occur. Fracture Management and Splinting tools, skills and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- Musculoskeletal Anatomy & Physiology
- Signs and symptoms of Strains
- Signs and symptoms of Sprains
- Signs and symptoms of Closed Fractures
- Signs and symptoms of Compound Fractures
- Signs and symptoms of Dislocations
- Principles of splinting
- Assessing and maintaining distal circulation
- How and when to apply cold to a bone, muscle or joint injury
- How to apply a low arm sling with a triangular bandage
- How to apply a high arm sling with a triangular bandage
- How to apply a cross-arm transport sling with a triangular bandage
- How to splint lower arm injuries
- How to splint upper arm injuries
- How to splint shoulder injuries and dislocations
- How to use a flexible foam splint (SAM splint)
- How to use speed straps for splinting
- How to splint a wrist injury with a SAM splint
- How to splint leg injuries
- How to splint knee injuries
- How to create a pelvic girdle to splint hip injuries
- Administration of Acetaminophen and Ibuprofen for pain management
.jpg)
According to the Public Health Agency of Canada, Heart Disease is the second most common cause of death for Canadians. When the arteries that feed the heart muscle itself become occluded or blocked with cholesterol, plaque or blood clots the muscles of the heart become starved of oxygen and cannot function properly. This can lead to chronic Chest Pain known as Angina, where the heart muscle is continually starved, and eventually cause a Myocardial Infarction (Heart Attack) where the heart muscle actually dies from lack of blood and oxygen.
In your Canadian Red Cross Emergency Medical Responder course, you'll learn how to recognize the most common signs and symptoms of a heart attack as well as the atypical/soft signs and symptoms mainly associated with heart attacks in women. In addition to taking the universal approach of treating for shock and keeping the person as calm, rested and comfortable as possible, you'll learn and practice how and when to administer Acetylsalycilic Acid (ASA/Aspirin) tablets which are platelet inhibitors and an anti-inflammatory, and Nitroglycerin spray which is a blood vessel dilator.
In circumstances where Nitroglycerin is contraindicated and chest pain persists, it may be appropriate to administer Nitrous Oxide (Entonox) to a heart attack patient for pain management. BC Emergency Health Services and BC EMALB have very specific, Provincially applicable parameters for the administration of these medications, including the ability to determine if Nitroglycerin can be given to someone without a previous prescription with remote medical oversight from Clini-Call's Emergency Physicians On-Call System (EPOS). Heart Attack, Angina and Myocardial Infarction management skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to recognize the signs and symptoms of probable Angina
- How to recognize the signs and symptoms of a probable Heart Attack
- How to recognize the "Soft" signs and symptoms of a probable Heart Attack
- How to identify and recognize the Indications to administer Nitroglycerin spray to a patient with a prescription
- How to identify and recognize the Contraindications to administering Nitroglycerin spray to a patient with a prescription
- How to identify and recognize the Indications to administer Nitroglycerin spray to a patient without a prescription
- How to identify and recognize the Contraindications to administering Nitroglycerin spray to a patient without a prescription
- How to administer Nitroglycerin spray to a patient experiencing signs and symptoms indicative of a Heart Attack
- How to identify and recognize the Indications to administer Acetylsalicylic Acid (ASA) to a patient experiencing signs and symptoms indicative of a probable Heart Attack
- How to identify and recognize the Contraindications to administering ASA to a patient experiencing signs and symptoms indicative of a probable Heart Attack
- How to identify and recognize the Indications to administer Nitrous Oxide (Entonox) to a patient for pain management
- How to identify and recognize the Contraindications to administering Entonox
- How to contact CliniCall / EPOS for remote medical directions
- How to provide assessment and care for a patient experiencing a probable Heart Attack
.jpg)
When a blood clot, embolism, plaque or aneurysm prevents adequate blood flow to the brain, a part of the brain tissue can starve or die, causing a stroke. In some cases the blood flow may resume before permanent damage occurs, which is commonly referred to as a Transient Ischemic Attack (TIA). The longer the blood flow is disrupted the more brain tissue dies and the more dramatic and permanent the damage becomes. As the left side of the brain controls the right side of the body, and the right side of the brain controls the left side of the body, the physical effects/deficits created by the stroke are usually seen on the opposite side of the affected brain.
Early recognition of the signs and symptoms of a potential Stroke, including sudden headache, one-sided weakness/paralysis, dizziness, confusion and slurred speech, and swift transport to definitive clinical medical care are the most important steps to prevent or mitigate permanent brain damage once a stroke has occured. When stroke-like signs and symptoms abate and resolve themselves shortly after ocurring, this is usually referred to as a Transient Ischemic Attack (TIA), however it is unlikely that you will be able to definitively diagnose between a Stroke and TIA on scene. The sooner a suspected Stroke patient gets to the hospital and receives advanced medical treatment and medications, the less brain function they will lose and the greater their chances of survival and fuller recovery. Stroke and Transient Ischemic Attack management skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to identify and recognize the signs and symptoms of a probable Transient Ischemic Attack (TIA)
- How to identify and recognize the signs and symptoms of a probable Stroke
- Field tools for assessing Stroke
- How to utilize and apply the Cincinnati Stroke Scale
- How to utilize and apply the F-A-S-T V-A-N Stroke assessment tool
- The importance of urgent transport for Stroke patients
- Positioning Stroke patients for transport
- How to provide assessment and care for a patient experiencing a probable Stroke or TIA
.jpg)
Every cell in the body requires a continuous supply of sugar (glucose) to function normally, with a greater demand for glucose accompanying greater exertion. The harder the body, and it's cells work, the more glucose they require. When our body digests food, many of the nutrients are broken down into glucose, which is subsequently absorbed into the blood stream for distribution to the cells. When cells require glucose, the pancreas releases an appropriate amount of insulin to facilitate transporting the approriate amount of glucose from the blood stream into the cells for energy.
Diabetes is a condition in which the pancreas is unable to produce either any insulin or enough insulin, or the cells are resistant to insulin as a glucose transporter. In Type I Diabetes, this condition is present from birth or early childhood, while Type II Diabetes develops later in life as an adult. Regardless of whether Type I or Type II Diabetes is present, the essential problem created is an imbalance of glucose and insulin available in the bloodstream compared to cellular demand for energy.
Many people with Diabetes of both types take synthetic insulin by injection, in an attempt to match glucose transport with cellular demand, but this is a very delicate balance requiring precise amounts compared to precise exertion levels. It is very common for someone with Diabetes to end up with blood glucose levels that are too low to support cellular function (Hypoglycemia) or blood glucose levels that are too high (Hyperglycemia) for the body to process efficiently. Of the two potential states, Hypoglycemia generally develops much more rapidly and is more immediately life-threatening.
In cases of suspected Diabetes, you will learn and practice how to measure the capillar blood glucose level (CapBgl) to determine if Hypoglycemia or Hyperglycemia is a factor in the patient's condition. Hypoglycemia is defined as CapBgl levels below 4 millimoles per liter (mmol/L), while Hyperglycemia is locally defined by BCEHS and BC EMALB as CapBgl levels above 11 mmol/L. If the patient is Hypoglycemic you will practice administering sugar/glucose gel when you can ensure that the patient will not choke on the substance. Diabetic Emergency management skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- The relationship between Insulin and Glucose
- The relationship between cellular function and blood glucose levels
- Type I Diabetes
- Type II Diabetes
- How to recognize the signs and symptoms of a Diabetic Emergency
- How to use a Blood Glucometer to measure Capillary Blood Glucose levels
- How to identify and recognize Hypoglycemia
- How to identify and recognize Hyperglycemia
- How to administer oral glucose to a patient experiencing confirmed Hypoglycemia
- How to provide care for an unresponsive patient with confirmed Hypoglycemia
- How to administer Glucagon to an unresponsive hypoglycemic patient by intramuscular injection (IM)
- How to administer Glucagon to an unresponsive hypoglycemic patient by instrasal spray (IN)
- How to provide assessment and care for a patient experiencing a Diabetic Emergency
.jpg)
Seizures can occur when the electrical signals travelling through and across the brain start to misfire or get re-routed to unintended destinations. There are many types of medical conditions and injuries that can lead to seizures including Stroke, TIA, Head Injury, Concussion, Epilepsy, Brain Tumors, Diabetes (Hypoglycemia), and Hyperthermia. Basically, anything that disrupts the normal function of the brain can potentially cause a seizure. With pediatric or infant patients in particular, it is very common for a high fever to induce febrile seizures.
Seizures usually take place through several different stages, which may or may not appear distinct and sequential. The "Aura" phase of a seizure most often manifests as strange sensation similar to deja vu, out-of-body or other sensations inconsistent with surroundings. Someone who has experienced a seizure before may recognize the sensations that accompany the aural phase and alert others to the impending event. The Tonic-Clonic phase of a seizure most often involves uncontrolled muscle convulsions and decreased responsiveness which usually last up to a few minutes. During the Tonic-Clonic phase, the seizing patient may also present with irregular breathing due to interference with the muscles involved in respiration, and vomit, foam or saliva accumulating in the mouth which can obstruct the airway. Seizures that last more than a few minutes, or seizures that occur back-to-back with no recovery time in between are referred to as Status Epilepticus and indicate an urgent medical emergency.
When the Tonic-Clonic muscle convulsions cease, the patient usually enters the Post-Ictal phase of the seizure during which they gradually regain consciousness, experience extreme fatigue and may or may not recall the previous moments leading up to and during the event. Some seizures, known as Focal Seizures do not involve muscle convulsions, but instead cause a period of trance-like decreased levels of responsiveness and can be more difficult to assess.
Regardless of the specific cause, your main patient care priorities during the tonic-clonic phase of a seizure involve taking whatever measures are necessary to create and maintain a safe space around the patient to reduce the risk of physical injury caused by the convulsions. In some cases you may need to move the patient away from a set of stairs or body of water to prevent a fall or drowning, but for the most part you will avoid physically contacting or restraining the patient until the seizure has concluded. Seizure management skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- Signs & Symptoms of Seizures
- Causes of Seizures
- Epileptic Seizures
- Status Epilepticus
- Phases of a Seizure
- Aural Phase of a Seizure
- Tonic-Clonic Phase of a Seizure
- Post-Ictal Phase of a Seizure
- Focal Seizures
- First Aid for Seizures
- Febrile Seizures
- Pediatric patients with high fever
- Patient care during a seizure
- Airway and respiratory concerns during a seizure
.jpg)
Burns are among the most painful type of injury, and are generally classified into 3 categories based on the depth of tissues affected. Superficial/First Degree burns only affect the outer epidermal layer of the skin, and are usually accompanied by painful reddened areas. Partial Thickness/Second Degree burns involve the deeper tissues of the dermis as well as the outer epidermal layers, and are generally identified by pain, blisters, redness and thick peels of skin. Full Thickness/Third Degree burns usually cause blackened, charred skin and tissue which may extend all the way down to the fatty layers, muscles and even bone.
Burns can become immediately life-threatening if they affect the airways and/or impair breathing, which is particularly common with inhalation injuries from being inside a burning building or breathing in chemical fumes. The most commonly life-threatening aspect of burn injuries is the rapid onset of infection and subsequent septic shock. This occurs because the skin which normally protects internal tissues and structures from infection is removed or damaged allowing bacteria to rapidly and overwhelmingly permeate the body's systems.
Some of the most important aspects of providing emergency medical care for burn injuries that you will learn and practice in your EMR course include ensuring your own safety (in particular when dealing with chemical or electrical burns), cooling the burn to prevent further tissue damage, and protecting the burned areas from infection with dry and sterile/clean dressings. Wet fabric will wick dirt and bacteria through to the tissues, so a burn is not protected unless the coverings are clean and dry.
One of the most effective methods to cool a burn, and therefore prevent the residual heat from creating more extensive burns to the surrounding tissues, is to apply cool, gently flowing sterile water or saline solution over the burned areas. Care must be taken not to further traumatize the damaged tissues, and ensure that the body core temperature is not lowered to a hypothermic state. Once the tissues have been cooled and the residual heat removed, the burn can be covered to prevent infection. BCEHS and BC EMALB stipulate Provincial emergency care regulations which limit the time spent cooling a burn on scene to 3 minutes, with any further cooling conducted in transport as appropriate. Burn Care skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to identify and recognize Superficial (First Degree) burns
- How to identify and recognize Partial Thickness (Second Degree) burns
- How to identify and recognize Full Thickness (Third Degree) burns
- The Rule of Nines for Adult patients
- The Rule of Nines for Pediatric patients
- Estimating Burn Percentage
- Burns requiring urgent transport
- Cooling a burn
- Covering burns to prevent infection
- Burn Dressings
- Burn Blankets
- Inhalation Injuries
- Pain management for burns
- How to provide assessment and care for a patient with burns
.jpg)
Trauma Management includes assessment and care for a wide range of physical injuries which can range from inconvenient and painful to immediately life-threatening. Very often the most urgent and critical aspect of a truamatic injury is not the most visible component, but the underlying interference with normal body system functions, or internal complications that can accompany the obvious physical damage. For example, the puncuture hole of a sucking chest wound may only be a few centimeters in diameter, with relatively minimal external hemhorrage but the increasing amount blood and air becoming trapped inside the pleural cavity of the chest wall create a tension pneumothorax which will eventually prevent the lungs from expanding and restrict heart contractions.
Some of the most common types of traumatic injury that you will learn about and practice treating in your EMR course include Sucking Chest Wounds, Peumothorax, Hemothorax, Crush Injury, Harness Syndrome, Compartment Syndrome, Pelvic Fracture, Flail Chest, Evisceration, Impaled Objects and Amputations. In almost all instances of these kinds of trauma, the underlying complications are usually more serious than the obvious external physical damage. Most of the immediate care that you provide for patients with truamatic injuries will focus on preventing further harm and mitigating the accompanying life-threatening complications.
You will learn and practice the application of a vented occlusive dressing over a sucking chest wound to mitigate the onset of tension pneumothorax, the application of a pelvic binder/girdle to prevent broken pelvic bones from lacerating abdominal organs during transport. Crush Injury and/or Harness Syndrome require a coordinated and rapid combination of extrication and immediate transport with supplemental intravenous fluids to counteract septic shock, while eviscerations require the application of multiple coverings over the exposed organs with a mix of absorbent, non-stick, moistened, non-permeable and insulatory layers. Traumatic Injury management skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to identify and recognize the signs and symptoms of an Amputation
- How to provide assessment and care for a patient with an Amputation
- Complete amputations
- Partial amputations
- How to identify and recognize the signs and symptoms of an Impaled Object
- Stabilizing an impaled object in place
- How to provide assessment and care for a patient with an Impaled Object
- How to identify and recognize the signs and symptoms of a suspected Pelvic Fracture
- How to create a pelvic girdle
- How to utilize a commercial pelvic binder
- How to provide assessment and care for a patient with a suspected Pelvic Fracture
- How to identify and recognize the signs and symptoms of an Evisceration
- How to provide assessment and care for a patient with an Evisceration
- How to identify and recognize the signs and symptoms of a Sucking Chest Wound
- Open Pneumothorax
- Closed Pneumothorax
- Spontaneous Pneumothorax
- Traumatic Pneumothorax
- How to provide assessment and care for a patient with a Tension Pnuemothorax
- How to identify and recognize the signs and symptoms of a Tension Pnuemothorax
- Tracheal Shift
- Jugular Vein Distension
- How to provide assessment and care for a patient with fractured ribs
- How to identify and recognize the signs and symptoms of fractured ribs
- How to provide assessment and care for a patient with a Flail Chest
- How to identify and recognize the signs and symptoms of a Flail Chest
- How to identify and recognize the signs and symptoms of Crush Injury
- How to identify and recognize the signs and symptoms of Harness Syndrome
- How to identify and recognize the Indications to administer Nitrous Oxide (Entonox) to a patient for pain management
- How to identify and recognize the Contraindications to administering Nitrous Oxide (Entonox)
.jpg)
The ongoing Opioid Overdose Crisis is one of the most lethal, large scale and persistent Canadian public health crises in the past few decades. With the recent deregulation of the Opioid Antagonist drug Naloxone (Narcan), many agencies have made emergency Narcan Overdose/Poisoning kits available to the public and especially the most vulnerable populations. Fentanyl / Carfentanil misuse comprises the vast majority of Opioid overdose and fatalities, but there are many other opiates and harmful drugs as well.
Administering Narcan, in either intramuscular or intrnasal form can temporarily alleviate the most life-threatening aspects of Opioid overdose, such as respiratory arrest and unresponsiveness, but it does not completely remove the poison from the person's system. The opioids will remain in the system after the Naloxone has dissipated, so it is vital that someone receives definitive clinical medical care as soon as possible following the overdose and subsequent Narcan administration.
The signs and symptoms of a patient who is experiencing Opioid Overdose/Poisoning will generally involve the "Toxidrome" of opioid overdose including decreased level of responsiveness, absent or inadequate respirations, and pinpoint pupils. The depressed respirations that typically accompany opioid overdose will also reduce the patient's blood oxygen levels (SpO2) to dangerously low levels. In most cases, you will place a higher priority on securing airway patency, supplementing their oxygen levels and assisting ventilations, or even performing CPR, than the immediate administration of Naloxone.
The administration of Naloxone, once appropriate, may further support these critical interventions by increasing the patient's level of conciousness and/or improving their natural respiration rate, rhythm and character. Although multiple doses of Naloxone, at increasing dosages, may be required for optimal patient care, it is not necessary to completely reverse all the effects of the opoiod or achieve full patient responsiveness, as long as the airway remains clear and adequate respirations resume.
As an Emergency Medical Responder you are also likely to encounter many other forms of poisoning and overdose such as household products, workplace chemicals, alcholol, barbituates, depressants, and stimulants which are not specifically related to opiates and therefore rendering Naloxone ineffective and contraindicated. Opioid Overdose and Poisoning skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- Types of Poisons
- Types of Drugs
- Types of Chemicals
- Household Products
- Workplace Chemicals
- Workplace Hazardous Materials Information System (WHMIS)
- Safety Data Sheets
- Poison Control Centers
- Ingested Poisons
- Inhaled Poisons
- Injected Poisons
- Absorbed Poisons
- Substance Misuse
- Substance Abuse
- Overdose and Poisoning
- Fentanyl and Carfentanil
- Opioid Overdose Crisis
- Deregulation of Naloxone
- Public Access NARCAN (Naloxone) Kits
- The Toxidrome of Opioid Overdose
- How to identify and recognize the general signs and symptoms of a suspected Overdose
- How to provide assessment and care for a patient experiencing signs and symptoms indicative of a suspected Overdose
- How to identify and recognize the signs and symptoms of an Opioid Overdose
- Intramuscular Naloxone (Narcan) Administration
- Intranasal Naloxone (Narcan) Administration
- Narcan / Naloxone doseages
- How to identify and recognize the Indications to administer Naloxone (Narcan) to a patient experiencing a suspected Opioid Overdose
.jpg)
The application of a SAGER Traction Splint is a specialized aspect of fracture management only utilized when the patient has a closed, mid-third femur fracture but no immediate life-threatening conditions. In the event that a patient shows signs or symptoms of any life-threatening injuries or conditions such as shock, decreased level of responsiveness, or respiratory distress in addition to a femur fracture the appropriate interventions include simple stabilization of the injuries and urgent transport initiated immediately following completion of the primary survey. Any additional assessment or interventions will take place enroute in the back of the ambulance.
If the SAGER Traction Splint is appropriate based the injuries and stability of the patient, you will learn and practice how to administer Entonox (unless contraindicated) prior to applying the traction, and then carefully position the splint to apply 1 pound of traction for every 10 pounds of patient body weight to a maximum of 15 pounds. Once applied, the amount of traction held by the splint, as well as the presence or absence of distal circulation must be diligently monitored and re-evaluated throughout patient care. If the injury is grossly deformed in a manner that impedes transport or inhibits distal circulation, it may be necessary to carefully move the leg back into anatomical alignment prior to application of the traction splint.
When properly applied, a traction splint can alleviate much of the pain from a femur fracture as well as preventing further interal tissue and blood vessel trauma by holding the fractured bone ends from grating against or sliding further alongside each other. Optimal patient care when utilizing a SAGER Traction Splint also involves careful stabilization of the injury throughout application, judicious placement of securing straps and adequate padding to ensure there are no hot spots or excessive movement on the affected leg. Transport of a patient wearing a traction splint will usually involve placement of a Robertson Orthopedic Stretcher (Clamshell) under the patient prior to lifting onto the cot. Traction Splinting skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to identify and recognize the signs and symptoms of a suspected Femur Fracture
- Open Femur Fractures
- Closed Femur Fractures
- Pediatric Femur Fractures
- Bilateral Femur Fractures
- How and when to properly apply a Sager Traction Splint for patients with a suspected mid-third Femur Fracture
- Femur Fractures involving the Hip or Pelvis
- Femur Fractures involving the Patella or Knee
- How to calculate the appropriate amount of traction
- How to properly place and secure the ankle brace above the malleolus
- How to proper place and the leg straps
- How to pull and read the traction meter
- How to ensure the splint saddle is properly oriented and placed against the ischial tuberosity
- How and when to administer Entonox prior to the application of a SAGER Traction Splint
- How to properly secure the figure 8 strap
- How to assess and reassess distal circulation and pedal pulses
- How to reassess the amount of traction held
- How to provide assessment and care for a patient with a suspected Femur Fracture
.jpg)
As an Emergency Medical Responder licensed through BC EMALB, one of your patient care duties will involve working with a Primary Care Paramedic or Advanced Care Paramedic and assisting them with intravenous therapy. Although endorsement to actually start an IV and inject a catheter into the patient's vein will require additional training and endorsement, you will be be permitted and required to maintain an existing IV Drip Set and calculate, calibrate and/or adjust the flow rate of the IV Fluids. This includes preparing the Drip Set delivery mechanism and spiking the IV bag to get the fluids moving through the Drip Set.
Drip Sets come in several different sizes, with Micro (Mini), Standard (Regular) and Macro (Adult) being the most common. The sizing of the Drip Set is based on the volume of each individual drip as it enters the chamber. A Micro Drip Set produces droplets of 60 gtts/ml, which means that it would take 60 of the droplets to make up 1 milliter (ml) of fluid, whereas a Macro Drip Set produces droplets of 10 gtts, which means it would only take 10 of these larger droplets to make up the same 1 ml of fluid. The larger the number, the smaller the individual droplets. You can adjust (titrate) how fast the drops move through the chamber, but the size of each droplet is pre-determined by the Drip Set and cannot be adjusted without changing to a different sized Drip Set.
The formula to calculate intravenous infusion times is: Drip Rate (Gtts per minute) = Volume to be Infused expressed in milliletres (ml) multiplied by Droplet Size expressed as drips per millilitre(gtts/ml) then divided by The allotted amount of Infusion Time expressed in minutes.
| Volume to be infused (ml) X Droplet Size (gtts/ml) | = Drip Rate (gtts/minute) |
| Infusion Time (minutes) |
Example: You are asked to infuse 500 ml of Normal Saline over the course of 120 minutes, using a Standard/Regular Drip Set with a droplet size of 15 gtts/ml.
| 500 ml X 15 gtts/ml | = 62.5 gtts/minute |
| 120 minutes |
The total of the top row (500 x 15) is 750, which is divided by the bottom row of 120 with a result of 62.5 drips per minute (gtts/minute). Rounding this result to the nearest practical, whole number you will titrate the Drip Set to 60 gtts/minute, or roughly 1 drip every second, moving through the drip chamber. This drip rate will intravenously infuse 500 ml of fluid over the course 120 minutes (2 hours). Note that the numbers in the above example are being utilized for purposes of illustrating the calculation process, and do not imply a prescribed clinical amount for any particular injury or condition.
You will learn and practice how to spike a bag of IV fluid, calculate the number of drops per minute necessary to deliver the amount of fluid prescribed over a set timeframe, and titrate the drip chamber to match the desired gtts/minute. Commonly utilize IV fluids contained in the sealed bags include Normal Saline utilized for general fluid replacement, D5W and D10W (Dextrose) used to increase blood sugar levels, Ringer's Lactate used to increase blood pressure to compensate for burns and trauma, and 2/3 -1/3 which contains a combination of Dextrose and Normal Saline. In addition to setting and monitoring the drip rates, you will also learn to detect and compensate for IV complications such as interstitial swelling and air embolisms. Intravenous Fluid and Drip Set Monitoring skills, tools and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- How to prepare and start an IV Drip Set
- How to calculate the correct flow rate for an IV Drip Set
- How to set, monitor and adjust the desired flow rate for an IV Drip Set
- How to identify and recognize the signs and symptoms of an Interstitial IV Complication
- How to provide care for a patient with suspected Interstitial IV Complication
- How to identify and recognize the signs and symptoms of a Circulatory Overload IV Complication
- How to provide care for a patient with suspected Circulatory Overload IV Complication
- How to identify and recognize the signs and symptoms of Thrombosis IV Complication
- How to provide care for a patient with suspected Thrombosis IV Complication
- How to identify and recognize the signs and symptoms of Thrombophlebitis IV Complication
- How to provide care for a patient with suspected Thrombophlebitis IV Complication
- How to identify and recognize the signs and symptoms of a Catheter Embolism IV Complication
- How to provide care for a patient with suspected Catheter Embolism IV Complication
- How to identify and recognize the signs and symptoms of a Site Infection IV Complication
- How to provide care for a patient with suspected Site Infection IV Complication
- How to identify and recognize the signs and symptoms of an Allergic Reaction IV Complication
- How to provide care for a patient with suspected Allergic Reaction IV Complication
- How to identify and recognize the signs and symptoms of an Air Embolism IV Complication
- How to provide care for a patient with suspected Air Embolism IV Complication
- How and when to discontinue an IV
.jpg)
Childbirth is a natural event which most often takes place as planned and predicted, without complications. However, when childbirth occurs ahead of schedule, unexpectedly, or under exigent circumstances, it can become one of the most stressful yet rewarding types of medical emergency you respond to as a paramedic or firefighter. Your EMR course and materials provides you with a basic understanding of childbirth, and how to provide medical assistance to the mother during labour and the birthing process.
You'll learn about pregnancy, and the stages of labour and childbirth, as well as universal steps to assist with delivery and make the mother, family members and newborn as comfortable and safe as possible throughout the birthing process. In the event of complications, you'll be familiar the most common underlying conditions which precipitate emergencies during the childbirthing process and which interventions are appropriate for each circumstance. Some of the most common pregnancy complications include spontaneous abortion, premature labour, ectopic pregnancy, and third trimester bleeding, and common childbirth complications include prolapsed cord, breech birth, limb presentation, and multiple births.
Once the newborn has been delivered, you will utilize the APGAR neonatal assessment system and provide any addtional care or intervention as required. In the event that a newborn (neonate) has a brachial pulse rate of less than 60 bpm, you will start CPR without an AED. The placenta will arrive within a few minutes of the infant, and should be kept warm and handled gently. The mother will also require care including interventions any ongoing or excessive hemorrhage. Emergency Childbirth tools, skills and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- Complications of Pregnancy
- Signs & Symptoms of Spontaneous Abortion
- Signs & Symptoms of Premature Labour
- Signs & Symptoms of Ectopic Pregnancy
- Signs & Symptoms of Third Trimester Bleeding
- The stages of Labour
- How to assess the stages of Labour
- Signs & Symptoms of Braxton Hicks Contractions
- Labour Stage One (Preparation)
- Labour Stage Two (Newborn Delivery)
- Labour Stage Three (Placenta Delivery)
- Labour Stage Four (Stabilization)
- The stages of the Birth Process
- How to assist with delivery of a baby
- Medical Complications of Emergency Childbirth
- Signs, Symptoms and Complications of Prolapsed Cord
- Signs, Symptoms and Complications of Breech Birth
- Signs, Symptoms and Complications of Limb Presentation
- Signs, Symptoms and Complications of Multiple Births
- Signs, Symptoms and Complications of Postpartum Bleeding
- How to provide medical care for a Neonate
- How to assess a Neonate using the APGAR systam
- Assessing Neonatal Alertness
- Assessing Neonatal Pulse
- Assessing Neonatal Grimace
- Assessing Neonatal Appearance
- Assessing Neonatal Respiration
- How to provide medical care for the Mother of a newborn
- Midwives and Doulas
- Planned and Unplanned Home Births
.jpg)
Although the phrases Multiple/Mass Casualty Incident (MCI) and Triage are often used interchangeably, they are distinct and separate terms. A multiple casualty incident describes any situation where two or more patients are injured, sick or otherwise require medical attention at the same time in the same vicinity. Vehicle accidents (particularly those involving passenger vehicles), hurricanes, tornados, earthquakes, building collapse, and chemical, biological radiological, nuclear, explosive (CBRNE) incidents are examples of circumstances that commonly create multiple casualty incidents. When patients/casualties outnumber available medical responders, Triage becomes necessary to avoid spending more time with any one patient than is absolutely necessary.
Triage is any rapid and efficient process of assessing multiple patients and quickly determining which require immediate care, which can wait, and which are already beyond saving. Most triage systems utilize a standardized color coding to identify four standardized patient categories. The color "Black" is utilized to identify patients who are already deceased or whose injuries are incompatible with life and will obviously outperform the available resources. The color "Red" is utilized to identify patients with immediately life-threatening injuries or conditions and for whom the application of critical interventions will create a more favourable outcome. The color "Yellow" is utilized to identify patients with injuries that are not immediately life-threatening but render the person unable/unsafe to move or walk without assistance. The color "Green" is utilized to identify patients who are uninjured, or whose injuries are not life-threatening and do not impede self-ambulation.
Color coding can be applied using a wide range of tools including markers, pre-coded tags, color coded flagging tape, color coded tarps, or spray paint to name a few. The assessment process utilized to rapidly determine which patient's are in which category is usually a variation of the primary assessment model, with strong emphasis on speed and efficency. In some cases, just calling out to a crowd and asking everyone who is capable to walk to a "Green" area may save time assessing patients without life-threatening injuries. In order to be effective, Triage depends on making instant decisions and spending only enough time with any given patient to ensure that they can sustain life a while longer. The more time that is spent on one patient, the longer another waits without assessment or treatment of any kind. It's important to keep in mind that Triage decisions are always extremely subjective and extended debate about any one decision defeats the purpose. It is also vital to maintain situational awareness and remain alert to new or unseen hazards related to the underlying causes of the multiple casualty incident. Multiple Casualty Incident and Triage tools, skills and principles covered in your Canadian Red Cross Emergency Medical Responder course and materials include...
- Factors in Multiple Casualty Incidents
- When patients outnumber rescuers
- When to initiate Triage
- Assigning a Triage Officer
- The START system of Triage
- Simple Triage and Rapid Treatment (START)
- Triage Assessment Model
- Colour Coding Tools
- How to identify triage patients who are deceased or beyond saving
- How to identify triage patients with immediately life-threatening injuries or conditions
- How to identify triage patients with non-life-threatening injuries
- How to identify triage patients who are unable to move themselves safely
- Chemical, Biological, Radiological, Nuclear, Explosive (CBRNE) events
- Emergency Wash-Down Procedures
- Incident Command System (ICS)
- Incident Management System (IMS)
- Multi-Agency Responses
.jpg)
Nobody would dispute that professional football and hockey players are exposed to exponentially more physical trauma on a daily basis than the average person. Correspondingly, these elite athletes also incur physical injuries at greater freqency and of greater severity than most. Therefore, professional athletes adopt disciplined regimens of preventative physical training and immediately seek physical therapy to restore normal function when injuries occur, in order to secure a long and healthy career. A professional athlete is not disqualified from competing simply because their bones are not unbreakable, nor are they stigmatized for sensibly seeking expert medical treatment to heal.
Professional medical responders must acknowledge that they are similarly exposed to exaggerated levels of emotional and psychological trauma, and take the same attitude and approach as professional athletes do towards prevention, treatment and self-care. Having frequent, normalized conversations about the normal reactions to abnormal situations and circumstances that first responders are exposed to on a regular basis, which challenge deeply held values, should be no different than discussing a broken ankle or sprained knee. Emergency responders should not expect themselves or others to be immune to the effects of mental stress any more than a football player is expected to have unbreakable bones.
Long term psychological health can be facilitated by adopting an overall healthy lifestyle that includes regular and sufficient sleep, proper nutrition and regular exercise accompanied by as much time as possible doing enjoyable activities with friends and family. It will also likely be necessary to acknowledge the presence of Occupational Stress Injury (OSI) and seek whatever professional resources are necessary to prevent long-term disability. You cannot take proper care of your patients (at least not for long) if you do not take responsiblity for and proper care of your own physical and mental health. A lifestyle that promotes long-term mental and physical wellness includes...
- Healthy eating habits that include a sensible balance of nutritional and dietary needs
- A structured and disciplined approach to sufficient sleep cycles
- Regular exercise and activities which build strength and endurance
- Normalized ongoing conversations about exposure to abnormal circumstances
- Ample and time with friends and family spent on enjoyable activities
- Maintaining current training and education to ensure you are performing your duties responsibly
- Ongoing education about Occupational Stress Injury (OSI)
- Professional counseling or medical assistance when needed
- Acceptance that you are not immune to stress
- Acceptance that recovery may not occur as quickly as you like
- Acceptance that everyone reacts differently to the same circumstances and that all reactions are "normal".
- Self-awareness of the signs and symptoms of cumulative or acute Occupational Stress Injury (OSI)
- Continuous and ongoing access to local, Provincial, Federal or employer specific Occupational Stress Injury resources
tel: 778-724-9054 email: training@mediprofirstaid.com
We recognize and respectfully acknowledge that we operate on the traditional and unceded territory of the Syilx Okanagan and Secwepemc peoples.

.png)
.png)
As a participant in a Canadian Red Cross Emergency Medical Responder course, you will need to work with and show respectful behaviour towards all of your classmates. Regardless of any personal, philosophical, religious or political differences, you must support each other's learning throughout the course.
Respect is particularly important when learning, practicing or performing skills that involve physical contact with another participant. Physical contact is an unavoidable component of many core professional medical responder skills, so participants must be as respectful and professional as possible during these segments.
Each participant will bring their own unique experiences, backgrounds and perspectives to your Emergency Medical Responder course, which will make the course more interesting and relevant for everyone, provided mutual respect is consistently demonstrated. Language or actions which impinge on every participants' right to a physically and psychologically safe learning learning environment will not be tolerated, and will result in expulsion from the program. You are not expected to agree with every aspect of your classmates' lifestyles and opinions, however you are expected to demonstrate respectful behaviour towards each other at all times.